Treating melanoma in the eye

People often associate melanoma with skin cancer that develops from exposure to ultraviolet (UV) light. However, a team of specialists at Houston Methodist Hospital have pioneered a way to treat a rare and relatively unknown type of melanoma that can occur in the eye: uveal melanoma.
Led by ocular oncologist and retina specialist Amy C. Schefler, M.D., assistant professor of clinical ophthalmology at Houston Methodist, the Ocular Oncology Team at Retina Consultants of Houston combines customized plaque brachytherapy (concentrated radiation), intraoperative ultrasound and genomic testing to treat patients affected by this rare form of melanoma.
“Over the last few years, particularly in the last five years since I’ve been here, … we’ve really upped our game in terms of the success of the procedure and a lot of the aspects of what we do,” Schefler said.
What is uveal melanoma?
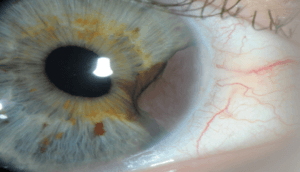
A close-up image of an eye affected with uveal melanoma. (Photo courtesy of Houston Methodist Hospital)
Uveal melanoma tumors are yellow or brown cells that form a mass in the tissue of the vascular layers of the eye behind the retina. Tumor masses range from 2 mm to 12 mm tall and 5 mm to 18 mm wide—no larger than the size of a jelly bean.
Studies estimate approximately 1,200 to 1,800 new cases of uveal melanoma each year in the United States. While some patients may experience floaters or blurry vision, most patients don’t exhibit any symptoms. They often discover the tumor during a routine eye exam and are surprised to learn that melanoma can develop in the eye, Schefler said.
The melanocytes, or pigment-producing cells, that travel to the eye live in a completely different microenvironment than the ones in the skin, Schefler said. Because they’re not exposed to the sun, they develop and behave differently than skin melanoma.
“[Uveal melanoma] is less related, believe it or not, to the degree of pigmentation because the sun doesn’t actually make it to the back of the eye. That’s what the role of the human lens is: to stop it,” Schefler explained. “When you look at the tissues in these tumors, genetically, they don’t have the typical mutations that you see in sun-exposed skin. There are typical mutations that sun causes: they cause mostly mutations in DNA repair mechanisms, but you don’t see that [with uveal melanoma]. These are not sun related.”
The exact causes for uveal melanoma are still unknown. No diet or environmental risk factors have been definitively linked to this type of cancer, but experts have found that uveal melanoma occurs mostly in patients who are Caucasian with lighter-colored eyes.
An eye-saving treatment approach
Traditionally, uveal melanoma was treated by surgically removing the eye, a procedure called enucleation. However, thanks to advances in biotechnology and radiation technology, uveal melanoma can now be treated without permanently removing the eye or loss of vision. Plaque brachytherapy treatment uses radioactive eye plaques that are customized to each patient’s tumor.

Examples of plaques with customized shapes and seed configurations. (Photo courtesy of Melvin Astrahan, Ph.D., and Eye Physics, LLC.)
The plaques, which are about the size and thickness of a quarter, are constructed out of pure gold on one side to protect the surrounding healthy tissue. On the side facing the eye are small radioactive “seeds” that emit radiation that travels through the wall of the eye to kill the tumor cells.
Because no two tumors are alike in size, shape and location, radiation oncologist Bin Teh, M.D., professor of radiation oncology at Houston Methodist, performs radiation calculations to determine the exact number and configuration of the radioactive seeds on the plaque for each patient.
“Our goal is to avoid the optic nerve and just truly plan to treat the tumor by [modifying] our dose exactly to the shape of the tumor,” Teh said.
Once the plaques are created, Schefler and her team surgically place the plaque on the outside surface of the eye, while performing a real-time ultrasound to make sure the plaque is centered. If the plaque is not accurately positioned, the part of the tumor that is not covered will regrow.
“We don’t leave the operating room until it’s perfectly centered,” Schefler said. “By doing that, we’ve had zero local recurrences … in the five years we’ve started our program here.”
The plaque is then left on the eye for a week. Once removed, the tumor cells have been eliminated, and the eye structure and vision are preserved.
In addition to plaque brachytherapy and real-time ultrasound, Schefler and her team perform genomic profiling on uveal melanoma tumors to assess a patient’s risk for metastases.
“Twenty years ago, if a patient came in, we would say, ‘Well, flip a coin, there’s a 50 percent chance you’ll live or die. We don’t know. Good luck,’” Schefler said. “But now … we do genomic profiling to figure out which patients are at higher risk of developing metastases from the disease and which aren’t.”
Using a microscope, special retinal instrumentation and a small needle, Schefler is able to extract microscopic amounts of cells from the uveal melanoma tumor to send off for genetic analysis, which classifies the melanoma into three different categories:
- Class 1A: Low risk of the tumor spreading
- Class 1B: Intermediate risk of the tumor spreading
- Class 2: High risk of the tumor spreading
“With rare cancers, we’re always playing catch-up because it takes longer for us to get funding …, but we’re finally reaching a threshold of really meaningful genomic data we can use to influence patient care,” Schefler said.
Schefler and Teh admit their multi-pronged approach of combining plaque brachytherapy, intraoperative ultrasound and genomic profiling—which usually takes three weeks from initial diagnosis to surgery—is time-consuming and labor intensive. But it has been proven to be more effective, with less collateral damage to the healthy parts of the eye.
“There’s no question that patients in our center do better than at other places because of the local control rate,” Schefler said. “But we want to get to a point in the next decade where even if we have 100 percent local control, if the patients’ genomics are such that there are a couple cells elsewhere, that we have therapy for that. That’s where the next level of science will come, and we’re working on that.”