Health Policy Course
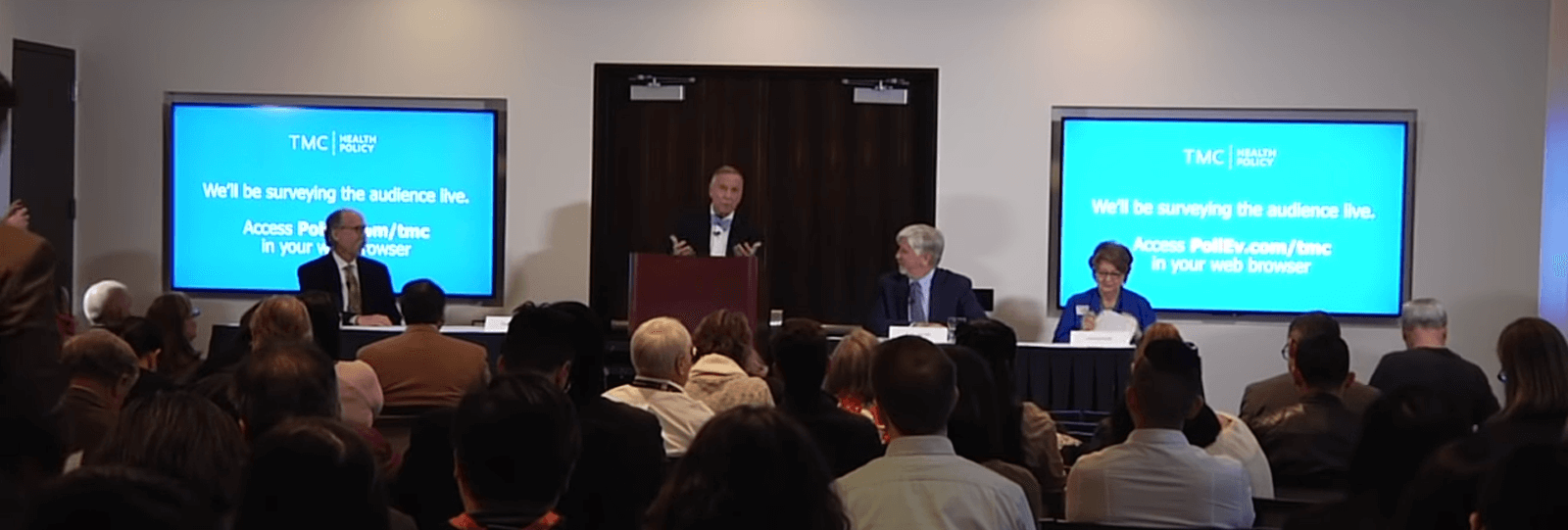
The TMC Health Policy Course is a first-of-its-kind collaboration between the Texas Medical Center’s academic institutions. The course, now in its second year, teaches students the fundamentals of U.S. health policy and provides them with the background and context they need to analyze the most pressing health policy challenges facing the country today.
The course includes 13 sessions organized by the TMC Health Policy Institute and led by experts from across the Texas Medical Center. The sessions complement students’ studies at their home institutions, from which they may earn course credit.
For more information on the course, contact Stephen.H.Linder@uth.www.tmc.edu.
 Play Button
Play Button
Video
Watch previously recorded sessions of the 2019 TMC Health Policy Course
Health Policy Course Partners



















Course Details
Course Directors:
Arthur Garson, Jr., MD, MPH, Director, TMC Health Policy Institute
Stephen H. Linder, PhD, Co-Director, TMC Health Policy Institute
Course Goal: The TMC Health Policy Institute Health Policy course will train teach students (participants) about fundamental key concepts related to the development, implementation, and evaluation of (U.S.) health policy in an innovative format.
Course Objectives: By the end of the semester, students will be able to:
- Describe the complex roles of the many participants in policymaking,
- Summarize and discuss key components of healthcare policy, and
- Assess competing positions on selected health policy controversies.
Course Overview: The TMC Health Policy Institute Health Policy course is an inter-institutional, inter-professional introductory health policy course for graduate students or advanced undergraduate students.
The Health Policy Institute will produce 13 seminar sessions (see topics below.) Each session will be led by an individual from a TMC member institution, and will select 3-4 others from TMC member institutions to participate in the seminar, to include diverse, inter-professional perspectives from local experts in the form of panel discussions, debates, and other interactive teaching modalities. Recommended pre-session readings will be provided ahead of time to course participants. The course is organized in three parts: (1) Policy Institutions and Processes (2) Policy Topics in US Health Systems issues (3) Emerging Topics & Controversies in Health Policy.
Course Leadership and Evaluation: Each participating institution will have a local course director who will be responsible for planning the course in terms of which TMC sessions to include (i.e. one institution may decide to include 10 TMC HPI course sessions and have 3 additional sessions of their own), and which additional readings, meetings, and other course work will be required. Assessment, evaluation, grading, and feedback will be entirely under the purview of the institution-specific course director and the institution’s curriculum committee.
Target Audience/Participants: This course is designed for students in all areas served by the TMC (such as nursing, pharmacy, medicine, PhD in research and advanced undergraduates); however, the TMC course will also be open to the public.
Cost: Free for participants
Steering Committee: Chuck Begley, Trevor Burt, Joslyn (Joey) Fisher, Tanweer Kaleemullah, Peggy Landrum, Jessica Mantel, Aisha Morris, Binata Mukherjee, Ben Raimer, Frances (Lee) Revere, Rocaille Roberts, Umair Shah, Abida Solomon, Sujit Sansgiry
Teaching Assistant: Adele Semaan
Communications Director: Ryan Holeywell
Course Directors
Students interested in obtaining course credit from their home institution for participation in the TMC Health Policy Course are encouraged to contact the appropriate faculty member listed below.
| Course Director | TMC Institution | |
|---|---|---|
| Cecilia Ganduglia Cazaban | Cecilia.M.GandugliaCazaban@uth.www.tmc.edu | UTHealth School of Public Health |
| Gloria Rose | gmrose@pvamu.edu | Prairie View A&M University |
| Sharisse Hebert | sahebert@pvamu.edu | Prairie View A&M University |
| John Prochaska | joprocha@UTMB.EDU | UTMB |
| Susan Ruppert | Susan.D.Ruppert@uth.www.tmc.edu | UTHealth School of Nursing |
| Nina Fredland | nfredland@twu.edu | Texas Woman’s University |
| Robin Toms | rtoms@twu.edu | Texas Woman’s University |
| Peggy Landrum | plandrum@twu.edu | Texas Woman’s University |
| Terry Kirk | tdkirk2@Central.UH.EDU | University of Houston College of Nursing |
| Isabelle Kusters | Kusters@UHCL.edu | University of Houston – Clear Lake |
| Aisha M. Moultry | morris_ma@TSU.EDU | Texas Southern University College of Pharmacy and Health Sciences |
