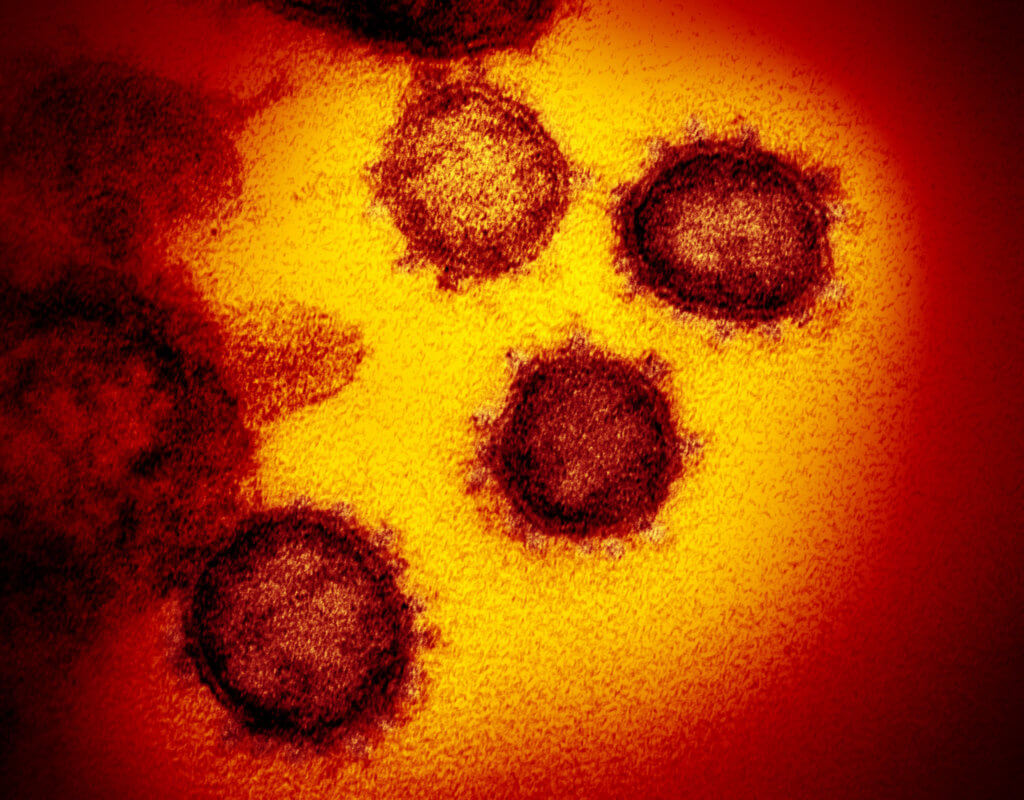
HIV and COVID-19: Two viruses collide

In 1981, reports began to emerge about a mysterious virus that caused illnesses, hospitalizations and deaths. Nearly four decades later, HIV/AIDS is recognized as a manageable chronic condition that remains powerful and pervasive enough to be classified as an epidemic, with close to 38 million people worldwide living with the virus. Significantly, we still don’t have a vaccine to prevent HIV/AIDS.
And now, COVID-19 presents a disproportionate threat to people with serious underlying health conditions.
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
Looking for the latest on the CORONAVIRUS? Read our daily updates HERE.
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
The current pandemic and the ongoing epidemic collided over the past few months to create new concerns for people living with HIV, concluded the 2020 International AIDS Conference, which wraps today online. Delegates from 175 countries attended the conference—the first virtual gathering of the world’s largest meeting on HIV—which had been set to convene in San Francisco and Oakland, California.
“The world faces an unprecedented emergency—the most lethal pandemic since AIDS emerged nearly 40 years ago. In recent months, COVID-19 has swept across the globe, bringing immense challenges, including for the tens of millions of people living with or affected by HIV,” stated a special report released by the International AIDS Society, which organizes the biennial global conference.
The report, “COVID-19 and HIV: A Tale of Two Pandemics,” outlines how COVID-19 has impacted HIV globally in three major ways: lockdowns have interrupted HIV treatment, care and prevention services; people in the lesbian, gay, bisexual, transgender and intersex (LGBTI) community are more vulnerable to HIV because of coronavirus; and COVID-19 has highlighted weaknesses in health care and supply chains that adversely affect people living with HIV.

Sandra Agola
Houston-area college student Sandra Agola, 26, helped plan the international conference as a member of the Global Village and Youth Programme Working Group.
Agola regularly offers advice for the Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN), a research program that aims to defeat the HIV epidemic among adolescents and young adults in the United States. ATN’s national advisory board, called Youth Experts and Advocates for Health (YEAH), focuses on prevention and care for young people with HIV.
“Our main goal is to help the researchers to basically create things the youth would be more attracted to, and with other things, like if they’re struggling with enrollment or diversity,” said Agola, originally from Nairobi, Kenya, who is an undergraduate studying health care wellness and navigation at the University of Houston-Downtown. “We have meetings and talk to a lot of different researchers and they ask our opinion about their studies. We tell them what we don’t like and what we think ought to be changed.”
Because of her experience as an ATN-YEAH member, Agola was chosen to review and rank abstracts that helped conference organizers select the research that was presented at the international program.
An estimated 1.2 million people in the United States have HIV, according to the Centers for Disease Control and Prevention.
Several thousand of those individuals receive treatment at Harris Health System’s Thomas Street Health Center, a freestanding HIV/AIDS clinic offering comprehensive care near the northwest edge of downtown Houston and one of the largest facilities of its kind in the United States.

Thomas Giordano, M.D., M.P.H.
To comply with social distancing standards, adjustments have been made over the last few months to continue care while keeping as many people physically away from the clinic as possible, said longtime Thomas Street medical director Thomas Giordano, M.D., MPH.
In addition to appointments via telemedicine—including video conferences and phone calls—prescriptions in larger quantities have been mailed to patients, he said.
Research is just beginning to emerge that investigates how these patients are faring amid COVID-19.
In late June, a study published online in Clinical Infectious Diseases found that people living with HIV who are admitted to the hospital with COVID-19 are no more likely to die than those who don’t have HIV—even though underlying health conditions associated with less desirable COVID-19 outcomes were more common in those who were HIV-positive.
“We found no differences in adverse outcomes associated with HIV infection for hospitalized COVID-19 patients compared to a demographically similar patient group,” the study concluded.
These findings mirror what HIV/AIDS experts in Houston have observed over the last four months.
The good news is that, generally, HIV patients with COVID-19 haven’t been any sicker than other patients, said Giordano, who is also professor and chief for the section of infectious diseases in Baylor College of Medicine’s department of medicine.
As we continue to wait for an HIV vaccine, more than 150 vaccines are being developed globally for COVID-19. In the United States, human COVID-19 vaccine trials are under way in several locations. The U.S. government has invested nearly $4 billion in “Operation Warp Speed” to make coronavirus vaccines and treatments available to Americans as soon as possible. Earlier this week, the federal government announced plans to pay $1.6 billion to vaccine manufacturer Novavax to expedite the development of 100 million doses of a COVID-19 vaccine.