COVID-19 has transformed the business of organ transplants

The COVID-19 global pandemic has slowed the transfer of vital organs for transplants. Testing for the disease caused by the novel coronavirus now extends to deceased persons who receive the same nasal swabs that make living patients flinch.
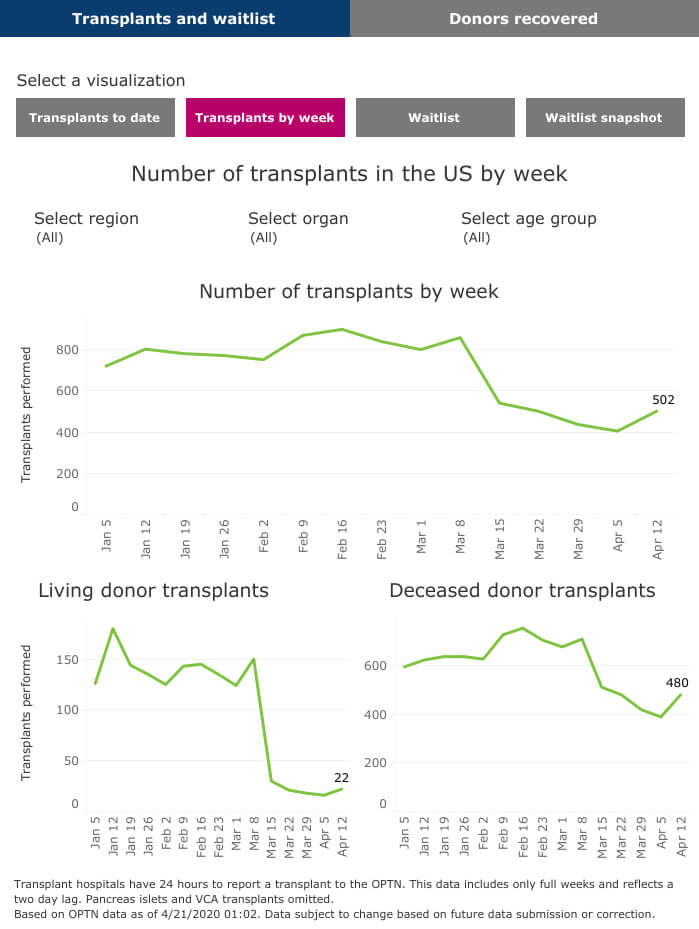
The public’s limited movement, thanks to stay-at-home orders and social distancing, means fewer of the accidents and other traumatic events that generate organ donation. Some people anticipating transplants have been inactivated, temporarily, from the national waitlist because of the coronavirus crisis.
Despite a dwindling supply, surgeons are declining organs from coronavirus hot spots. In addition, concern about the availability of personal protective equipment (PPE) has halted live donor transplants at local transplant centers.
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
Looking for the latest on the CORONAVIRUS? Read our daily updates HERE.
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
“We are not recovering organs and transplant centers are not transplanting organs from donors who have positive tests for COVID-19,” said Kevin Myer, president and CEO of LifeGift, a Houston-based organ procurement organization that serves 109 Texas counties and more than 200 hospitals, including transplant centers in the Texas Medical Center. “Depending on where you are in the country—obviously in New York and Seattle and in other places—transplantation slowed down, but it didn’t stop and it still hasn’t stopped.”
The prospect of eclipsing 2019—a record year for organ donations and transplants in the United States—may be fading as COVID-19 cases continue to rise across the country.
Still, the transplant community maintains hope, for now, especially because April is National Donate Life Month.

LifeGift President and CEO Kevin Myer
New procurement procedures
As part of the new pandemic procedure, a potential donor’s next-of-kin is questioned about the person’s travel history as well as exposure to various diseases and infections, including the novel coronavirus.
“We are recovering a sample, a nasal swab, for COVID-19 testing,” Myer said, adding that the additional process with test results in about 24 hours began in mid-March. “If we get a positive test back, we would stop the case.”
Other adjustments in the acquisition of organs include restricting travel. Typically, a LifeGift perfusionist and transplant surgeons recover an organ in person. Now, operating surgeons depend on their capable counterparts to match an organ in one place to a patient in another.
The shift has affected LifeGift’s donor and transplant tallies, which dropped by about half from February to March.
“For March, we recovered 31 organ donors and transplanted 97 organs. For us, that’s a little bit lower than what we typically do in a month, but we did not experience the massive drop some other areas have had. For tissue donors, we are also very close to what we planned for March,” Myer said. “For our whole first quarter, we are right on track. Part of the reason for that is that you had the busiest level of activity that we ever had. We recovered 54 organ donors and transplanted about 186 organs in February.”
Transplant centers adjust
After attending a late-February transplant conference in Phoenix where a Canadian colleague left early because of his country’s public health emergency, J. Steve Bynon, M.D., chief of abdominal transplantation at Memorial Hermann-Texas Medical Center, returned to Houston and assembled his team to discuss COVID-19.
“I said: ‘This is going to be a major problem. We need to not expose our patients. We don’t know who has it and who doesn’t; that’s one of the problems without extensive testing. We need to cancel all of our post-transplant clinics because those people are immunosuppressed and we don’t want to expose them, potentially, to other people who have it,’” Bynon recalled.
The hospital turned to telemedicine options for recently discharged transplant patients. Live transplants were canceled to save PPE and ventilators.
“When you have a health care crisis like this, you have to change gears very quickly and conserve resources,” Bynon said. “We decided we would not take organs from areas of the country that had high incidences of COVID. We would not take any organs from donors that we thought would be high risk from their method of death, such as unknown respiratory illness. Now, every donor is tested for COVID. Between those three criteria, we make a decision about whether we would accept those organs or not.”

Steve Bynon, M.D., left, chief of abdominal transplantation at Memorial Hermann-Texas Medical Center, performs surgery.
Transplant candidates are also screened with nasal swabs. Both donors and recipients also may receive a bronchoscopy, an endoscopic visualization of the airways, as well as a chest CT scan that might reveal COVID-19 characteristics in those who are asymptomatic.
A month passed before the Memorial Hermann team could get rapid COVID-19 testing on donors. Even then, tests are sensitive about 70 percent of the time, “so you are missing about 30 percent of the infections,” Bynon said. “The more information you have, the better decisions you can make to make it as safe as possible for your patients.”
He has participated in conference calls to share ideas with other TMC surgeons including Osama Gaber, M.D., director of the J.C. Walter Jr. Transplant Center at Houston Methodist; John Goss, M.D., director of liver transplantation at Baylor St. Luke’s Medical Center; and Christine O’Mahony, M.D., surgical director of kidney transplantation at Baylor St. Luke’s and the Michael E. DeBakey VA Medical Center. Goss and O’Mahony are also on the transplant teams at Texas Children’s Hospital.
Bynon, who is also a professor of surgery at The University of Texas Health Science Center at Houston (UTHealth) McGovern Medical School, has been tethered to an international online discussion of “fascinating” threads, he said, from transplant surgeons around the world—particularly those in Italy and China. He’s up at 5:30 every morning reading their dispatches and advice, then jumps back online after dinner.
“That kind of ready access to information is vital for your patients,” he said. “We have a lot of unknowns.”
LifeGift still operating
Donors and transplants reached all-time highs in 2019, according to the United Network for Organ Sharing (UNOS), the nonprofit that manages the country’s organ transplant system under contract from the U.S. government.
So far in 2020, transplants nationwide declined in mid-March and began to fall behind last year’s record trajectory in early April.
While the number of weekly transplants nationwide hovered around 800 for the first two months of 2020, that number dipped to between 400 and 600 per week by the middle of March.
Myer expects the local numbers to remain lower until the summer.
“We think that our activity levels will actually drop off in April and May and then we think in June and July things will come back up and, by July, we will be back to a new normal,” he predicted.
For now, the LifeGift call center and other vital operations are remote but fully operating. LifeGift continued working through Hurricane Harvey in 2017, Myer noted, and has done so through this disruption as well.
“We have a virtual platform. Our call center is fully remote. A lot of our staff who do hospital development are doing that virtually to minimize traffic in and out of the hospitals,” he said. “People still want to donate. People are in the hospitals counting on us right now. That whole concept of ‘we offer hope’ is probably more true now than ever.”