Coronavirus: A Texas Medical Center continuing update

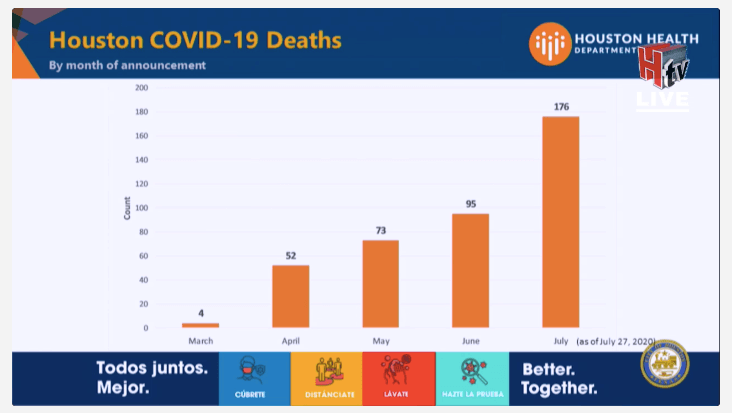
UPDATE | September 15, 2020, 4:30 p.m.: Houston Mayor Sylvester Turner tweeted today’s updated COVID-19 numbers for the city. There were 325 news cases today, bringing the city’s total to 69,567. In addition, there were 12 newly reported deaths, bringing Houston’s total to 982.
COVID-19 deaths of children under 21
A new report from the Centers for Disease Control and Prevention found that 121 people under age 21 in the United States died of COVID-19 between Feb. 12 and July 31, 2020.
Of those deaths, 78 percent occurred among Black, Hispanic and American Indian/Alaska Native individuals. Twelve were infants and 85 were aged 10 to 20 years.
Although symptoms associated with COVID-19 are milder in children than adults, the report concluded that “ongoing surveillance for SARS-CoV-2-associated infection, hospitalization and death among persons aged <21 years should be continued as schools reopen in the United States.”
COVID-19 and blood group
STAT News reported this week that a study forthcoming from 23andMe, the personal genomics and biotechnology technology company known for its direct-to-consumer DNA test, shows that an individual’s “genetic code could be connected to how likely they are to catch Covid-19—and how severely they could experience the disease if they catch it.”
The 23andMe study, which included web-based surveys of more than one million research participants, found that people with blood group O tested positive for COVID-19 less frequently than people with other blood groups.
At least one previous study came to a similar conclusion in terms of blood group.
The 23andMe study also found that African American ancestry, obesity, lower socio-economic status and pre-existing conditions were associated with a higher risk of hospitalization in COVID-19 patients.
The new study, Stat News reported, has not yet been peer-reviewed.
Role reversal
The New England Journal of Medicine today published a “Perspective” piece about the role reversal of Big Pharma and the U.S. government, “Up Is Down—Pharmaceutical Industry Caution vs. Federal Acceleration of Covid-19 Vaccine Approval.”
The article references the Sept. 8 pledge from nine pharmaceutical companies saying they would not apply for approval of a COVID-19 vaccine until they were satisfied that data from clinical trials was adequate.
“From a legal perspective, the CEOs’ pledge to hold back on seeking marketing permission prematurely could lead to the unusual situation of the government advocating for quick approval of a medical product even as its manufacturer declines to request such approval,” states the article, written by members of Brigham and Women’s Hospital and Harvard Medical School, both in Boston. “Then what? The FDA process is predicated on a sponsor submitting an application to the agency. But an administration that has taken an unprecedented role in influencing FDA policy on COVID-19 could encourage the agency to issue an EUA [Emergency Use Authorization] for a product that has antibody data that only seem promising, even without a formal approval request by its manufacturer.”
The article looks ahead to the coming months, noting that the federal response to public distrust and the nine pharmaceutical companies “will help determine not just the fate of the first COVID-19 vaccines, but also what remains of the public’s eroding trust in one of the most important aspects of U.S. science policy.” — Maggie Galehouse
UPDATE | September 14, 2020, 3:45 p.m.: Yesterday, the World Health Organization (WHO) reported the highest single-day increase in global infections since the pandemic began, with 307,930 new cases. The previous daily high was on September 6, with 306,857 new cases.
The Houston Health Department is reporting today 329 new cases of COVID-19 and 7 additional deaths, bringing the city’s totals to 69,242 cases and 970 deaths. During an afternoon press briefing, Mayor Sylvester Turner also announced that the city’s positivity rate had dropped to 6.1 percent, but reiterated that the goal was for the rate to drop below 5 percent.
“This virus is still very much present, we need to be very, very vigilant—even though the positivity rate is moving in the right direction, it can easily go up just like it is coming down,” Turner said.
Another positive metric: according to the Houston Chronicle, the percentage of Houston-area ICU patients hospitalized for COVID-19 fell to 14 percent on Sunday, the first time that percentage has fallen below 15 percent since May 31. The drop is “a key achievement that indicates the virus is slowly being brought under control here,” the authors of the article wrote.
During today’s press conference, Turner also announced the expansion of the Mayor’s Office of Human Trafficking to include efforts around domestic violence. The newly named Mayor’s Office of Human Trafficking and Domestic Violence will continue to focus on gender-based violence and will expand its focus on domestic violence issues, which have escalated during the pandemic.
“We know that the stresses created by the COVID-19 pandemic have increased the risk for domestic violence, sexual assault and abuse for women and girls nationwide,” Turner said. “COVID-19, let me quickly say, is no excuse for any kind of domestic violence or abuse.”
Turner added that in the last few months, service agencies have reported a large uptick in requests; he said the Houston Area Women’s Center reported a 40 percent increase in calls and Aid to Victims of Domestic Abuse reported a 90 percent increase for protective orders. Turner said that while there are complexities to this issue, the office will begin by focusing on the financial and economic abuse that survivors often experience.
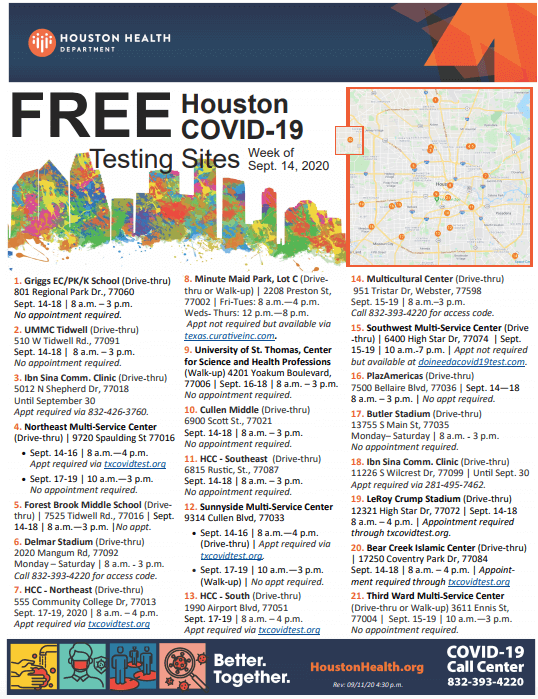
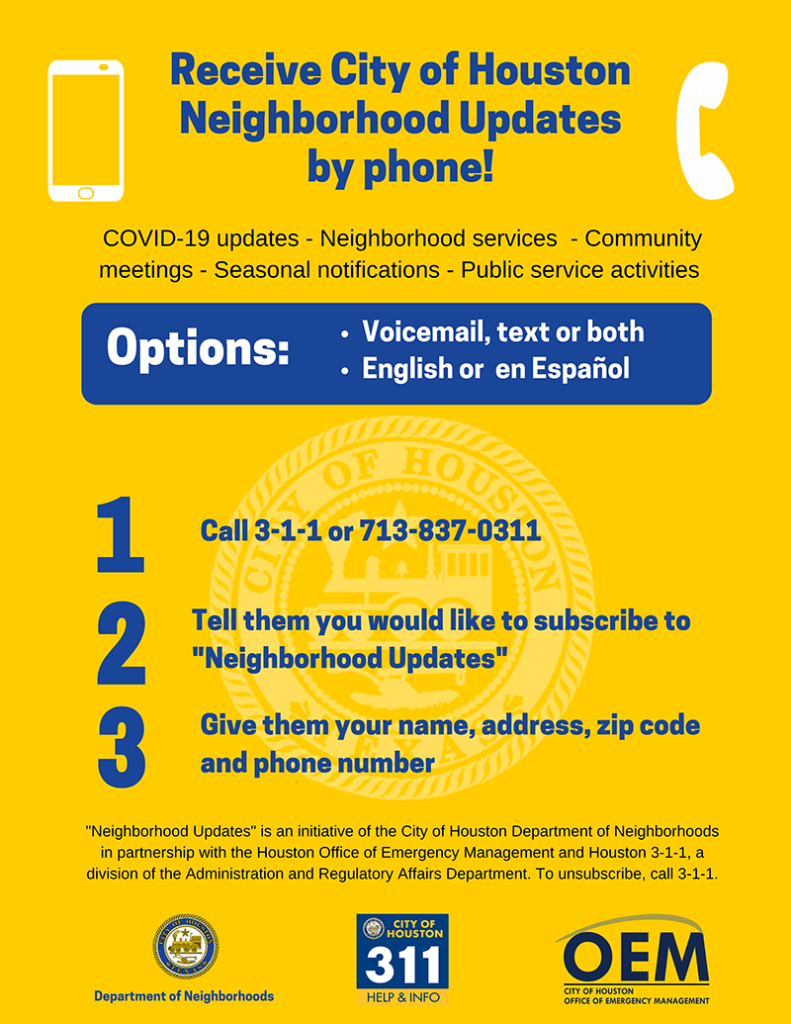
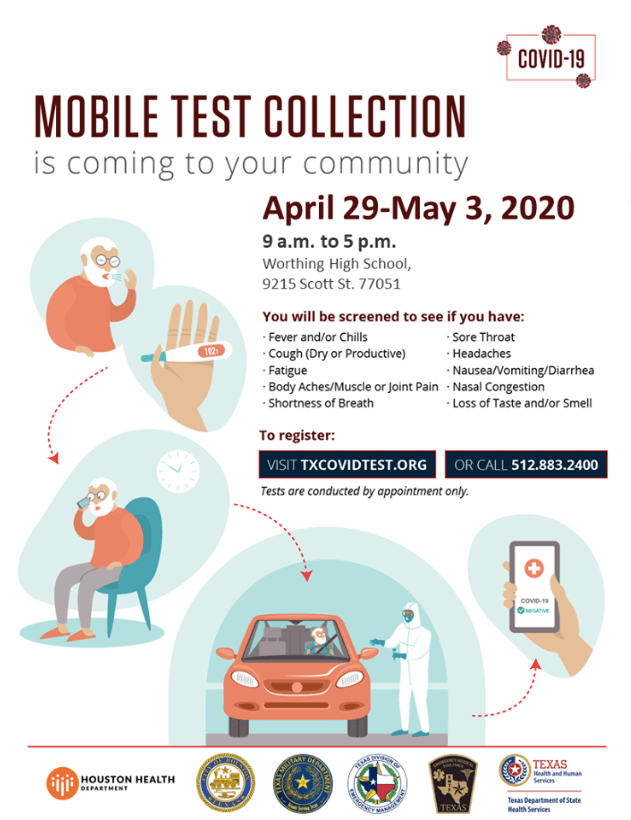
The Houston Health Department and its partners have also announced the schedule for free COVID-19 testing sites throughout the city this week.
The Harris County Agency on Aging is also offering in-home COVID-19 testing for homebound individuals, including those with disabilities and adults 60 years and over. Inquiries can be made at 832-393-4301 or 800-213-8471.
In COVID-19 vaccine news, AstraZeneca has resumed the Phase 2/3 trial for its vaccine candidate in the United Kingdom only. The trial was suspended temporarily after one of the trial participants experienced a potential adverse reaction involving inflammation of the spinal cord. The testing has not yet resumed in the United States, Brazil and South America, where AstraZeneca is also conducting Phase 2/3 and Phase 3 trials. In addition, Pfizer and BioNTech are hoping to expand their Phase 3 trail for their COVID-19 vaccine. The move will require FDA approval, but the companies hope to increase their participant size from 30,000 to 44,000 individuals. And, according to China’s top medical official, the country will not work to vaccinate its entire population against COVID-19 once a vaccine is available, but prioritize frontline workers and vulnerable populations.
Finally, Baylor College of Medicine released today a set of guidelines for schools across the country to reference as they make plans to reopen.
“Baylor has a history of working closely with math and science-focused schools in Houston and South Texas,” Paul Klotman, M.D., president, CEO and executive dean at Baylor, said in a statement. “We feel strongly that we should share broadly our expert guidance on how and when to open schools safely in this time of pandemic.”
The guidelines address a wide range of topics, including decisions related to reopening timelines and planning and preparing for re-entry; planning for physical distancing; attention to facilities, including how to clean and disinfect; health supplies; guidance on face coverings, classroom spacing and reducing interactions among students; communication efforts; screening and testing students and teachers for COVID-19 symptoms; potential exposure and protocols for positive cases; and isolation and quarantine instructions. — Alexandra Becker
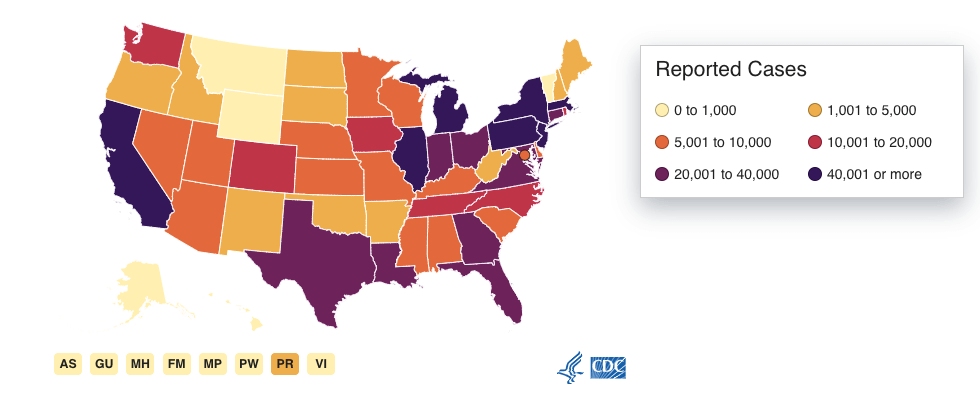
UPDATE | September 11, 2020, 3:30 p.m.: On this 19th anniversary of 9/11, as we remember the nearly 3,000 people who perished in New York City, Pennsylvania and Washington, D.C., the Johns Hopkins Coronavirus Resource Center reported the following national numbers for COVID-19 in the United States:
- 6,397,000 total cases
- 35,286 new cases
- 191,800 total deaths
- 907 new deaths
For daily updates of national numbers, visit the “Data in Motion” feature on the Johns Hopkins website.
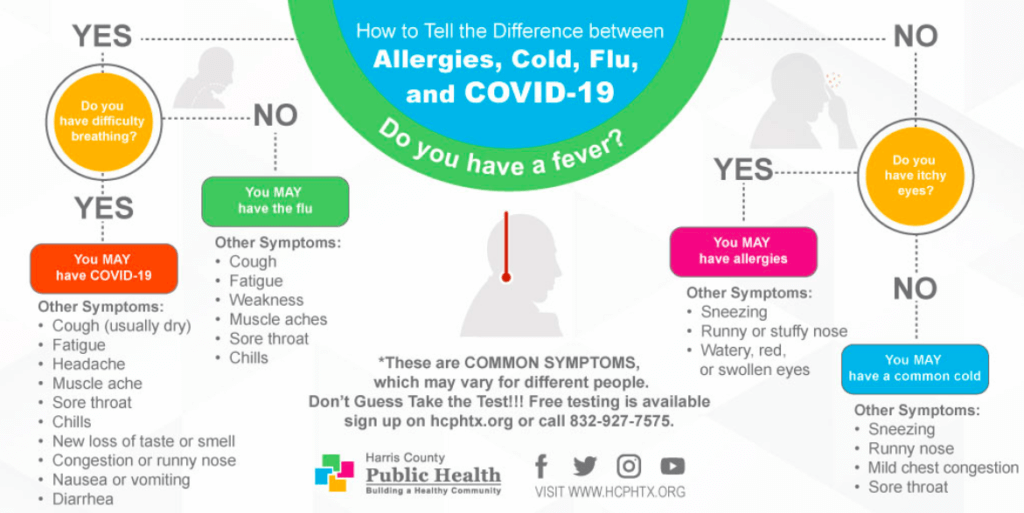
Allergies, cold, flu or COVID-19?
Flu viruses are most common during the fall and winter, with influenza activity ramping up as early as September and October. As we head into the weekend, a graphic released this week by Harris County Public Health might help people sort out several symptoms they may be experiencing.
N95 masks in short supply
The Associated Press reported Thursday that medical supplies needed to battle COVID-19 remain in short supply, despite the fact that White House officials say U.S. hospitals have all the supplies they need. N95 masks are among those items experiencing critical shortfalls in certain places.
“Front-line health care workers, hospital officials and even the Food and Drug Administration say shortages persist,” the AP story said.
The White House took too long to sign contracts with companies that produce “meltblown textile,” the dense mesh made from plastic that allows N95 masks to block small particles—including viruses, according to the story.
The report is “part of an ongoing investigation by the Associated Press, the PBS series “Frontline” and the Global Reporting Centre that examines the deadly consequences of the fragmented worldwide medical supply chain.”
U.S. government adjusts entry strategy for international air passengers
Starting Sept. 14, the U.S. government will stop the enhanced entry health screening for passengers arriving from China, Iran, the Schengen region of Europe, the United Kingdom, Ireland and Brazil.
“We now have a better understanding of COVID-19 transmission that indicates symptom-based screening has limited effectiveness because people with COVID-19 may have no symptoms or fever at the time of screening, or only mild symptoms,” a media statement posted on the Centers for Disease Control and Prevention website said. “Transmission of the virus may occur from passengers who have no symptoms or who have not yet developed symptoms of infection. Therefore, CDC is shifting its strategy and prioritizing other public health measures to reduce the risk of travel-related disease transmission.”
Going forward, government resources will focus on individual passengers and a series of new initiatives, including robust illness response at airports; voluntary collection of contact information from passengers using electronic means; potential testing to reduce the risk of travel-related transmission of the virus that causes COVID-19; country-specific risk assessments to assist passengers in making informed decisions about travel-related risk; and post-arrival passenger recommendations for self-monitoring and precautions to protect others. — Maggie Galehouse
UPDATE | September 10, 2020, 3:30 p.m.: An increasing body of research has been published to shed light on the specific ways COVID-19 has roiled the United States for more than six months. Two papers published today explain how the novel coronavirus has caused people to delay care and its disproportionate weathering on poor individuals and people of color.
“Beyond the Case Count: The Wide-Ranging Disparities of COVID-19 in the United States” from The Commonwealth Fund concluded that “COVID-19 pandemic’s impact in the United States has exposed long-standing inequities by race, ethnicity, and income.”
The results are an analysis of the U.S. responses to the Fund’s 2020 International Health Policy COVID-19 Supplement Survey, fielded in the U.S. and nine other countries from March 30 to May 25, 2020.
Of the report’s U.S. findings:
- More than half of Latino and nearly half of Black survey respondents reported experiencing an economic challenge because of the pandemic, which is substantially more than the 21 percent of white respondents.
- Thirty-nine percent of women reported significant mental health concerns related to COVID-19 — 13 percentage points higher than men. For people with low incomes, the rate of mental health concerns was nearly 20 points higher than the rate for people with high incomes.
- Both Black and Latino respondents reported pandemic-related mental health concerns at a rate approximately 10 points higher than whites.
- Compared to health care providers, state and local officials and President Trump received lower marks for their responses to the pandemic. Black survey respondents held the least favorable views of government leaders’ actions.
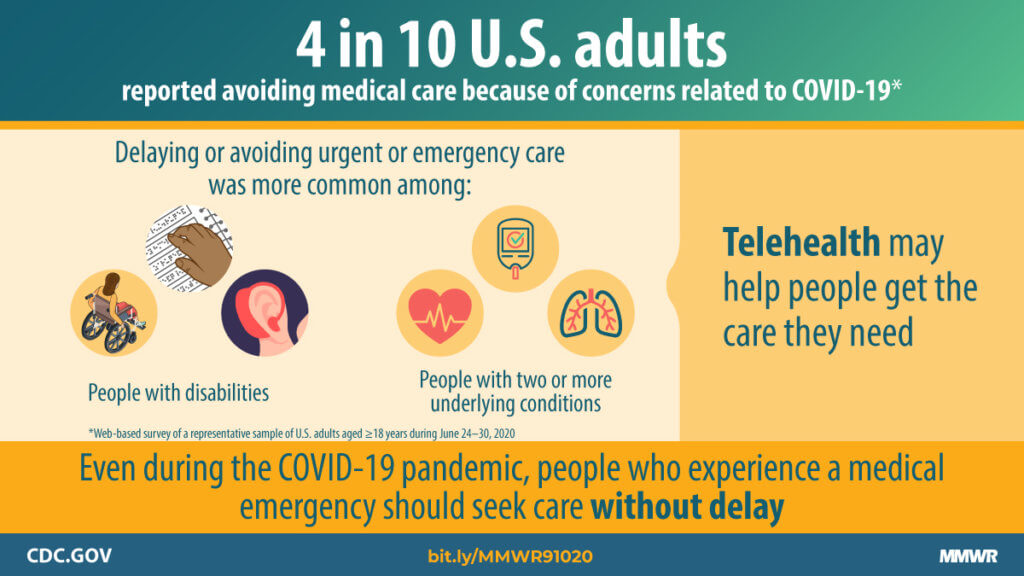
Also, the Morbidity and Mortality Weekly Report from the Centers for Disease Control and Prevention (CDC) issued results of a survey showing that an estimated 41 percent of U.S. adults have avoided medical care during the pandemic because of concerns about COVID-19, including 12 percent who sidestepped urgent or emergency care and another 32 percent who bypassed routine care.
This confirms the anecdotal concerns of Houston-area clinicians and the health care executives who have warned about decreased traffic for preventive care including vaccinations, annual well exams and screenings such as mammograms and colonoscopies.
“These findings align with recent reports that hospital admissions, overall emergency department (ED) visits and the number of ED visits for heart attack, stroke, and hyperglycemic crisis have declined since the start of the pandemic, and that excess deaths directly or indirectly related to COVID-19 have increased in 2020 versus prior years,” the report said. “Nearly one third of adult respondents reported having delayed or avoided routine medical care, which might reflect adherence to community mitigation efforts such as stay-at-home orders, temporary closures of health facilities, or additional factors. However, if routine care avoidance were to be sustained, adults could miss opportunities for management of chronic conditions, receipt of routine vaccinations, or early detection of new conditions, which might worsen outcomes.” — Cindy George
UPDATE | September 9, 2020, 3:40 p.m.: The Houston Health Department reported today 223 new cases of COVID-19 and eight new deaths, bringing the total to 66,488 cases and 906 deaths. In addition, the city’s positivity rate is 6.6 percent.
Houston to begin restarting live events
Houston Mayor Sylvester Turner announced today that he will allow live events with certain health and safety protocols in place, starting with small audiences that fill 25 percent of a controlled venue’s normal occupancy.
The Houston Symphony, which typically seats 3,000, will allow 150 guests to attend a concert series at Jones Hall. The Houston Dynamo and Dash have also announced that they will begin hosting their games with less than 25 percent capacity in BBVA Stadium.
However, parades, fun runs, walks, biking events, festivals and other similar events in uncontrolled spaces or venues will continue to be on hold through the rest of the year.
Houston mourns death of HFD Captain Tommy Searcy
Houston Fire Department Capt. Tommy Searcy died yesterday due to complications from COVID-19.

Houston Fire Department Capt. Tommy Searcy (Courtesy photo)
“Capt. Searcy fought his illness with the same fierce bravery that he exhibited throughout his 18-year HFD career. Searcy’s family, HFD Chief Sam Peña, and fellow firefighters will undoubtedly miss his leadership and dedication to the fire department,” Turner said in a statement.
A father of three daughters, Searcy, 45, was the third HFD firefighter to die in the line of duty as a result of the novel coronavirus. HFD veteran Jerry Pacheco and Capt. Leroy Lucio also perished.
Searcy was given the experimental drug, RLF-100, also known as aviptadil, on Aug. 19, after members of HFD fought to cut through red tape to get the drug from Houston Methodist to Memorial Hermann in the Woodlands, where Searcy was being treated.
NeuroRx, the company that manufactures the RLF-100, said that the drug improved recovery from respiratory failure in most critically ill COVID-19 patients. The U.S. Food and Drug Administration granted RLF-100 a Fast Track designation, which allows companies to expedite the review and development process. In collaboration with the National Institutes of Health, RLF-100 is undergoing development as a Material Threat Medical Countermeasure.
“Tommy’s death is a reminder to be vigilant in our efforts to keep our families, friends, and station crews safe in the face of the COVID-19 pandemic,” Houston Professional Fire Fighters Association president Patrick “Marty” Lancton said in a statement.
AstraZeneca stops COVID-19 vaccine study due to suspected adverse reaction
AstraZeneca and the University of Oxford’s Phase 3 clinical trial for a COVID-19 vaccine was halted yesterday due to a suspected serious adverse reaction in one of the participants at a United Kingdom testing site.
According to STAT News, the participant experienced neurological symptoms associated with transverse myelitis, a rare spinal inflammatory disorder. Her condition is currently improving and she will be discharged Wednesday, but no official diagnosis has been made yet.
“As part of the ongoing randomized, controlled global trials of the Oxford coronavirus vaccine, our standard review process was triggered and we voluntarily paused vaccination to allow review of a safety data by an independent committee,” an AstraZeneca spokesperson wrote in a statement. “We are working to expedite the review of the single event to minimize any potential impact on the trial timeline. We are committed to the safety of our participants and the highest standards of conduct in our trials.”
AstraZeneca’s clinical trial is one of nine vaccine candidates currently undergoing Phase 3 studies. The study, which is being done at 62 sites in the United States, started on Aug. 17 and was estimated to complete collecting final data in December 2020; however, it is unclear how long AstraZeneca’s study will be on hold.
New polls shows financial impact of the pandemic on American households
New nationwide polls found that more than half of the households in four major U.S. cities including Houston are experiencing financial issues, highlighting the widespread burden and disparate impact of the COVID-19 pandemic.
NPR, the Harvard T.H. Chan School of Public and the Robert Wood Johnson Foundation (RWJF) conducted a series of polls, titled “The Impact of Coronavirus on Households in Major U.S. Cities,” to better understand the effects of the pandemic. Researchers collected responses about household finances, employment, health care, housing, transportation and well-being from 3,454 adults age 18 or older between July and August 2020.
The results showed that households in Chicago (50 percent), New York City (53 percent), Los Angeles (56 percent) and Houston (63 percent)—primarily those in Black and Hispanic communities—reported financial troubles, such as depleted savings and difficulty paying bills or affording health care.
Households in New York City (59 percent), Los Angeles (63 percent), Chicago (55 percent) and Houston (75 percent) reported experiencing negative health consequences as a result of an inability to access care when needed.
“This pandemic has revealed glaring problems in the nation’s health care system,” RWJF president and CEO Richard Besser, M.D., said in a statement. “At a time when a significant number of people need health care most, many cannot get it. We need to be able to provide safe, affordable care for people with COVID-19, as well as for the many with chronic medical conditions so rampant in America. It is unacceptable that in a wealthy nation like ours factors such as income or race play such a big role in health care access.” — Shanley Pierce
UPDATE | September 8, 2020, 2:30 p.m.: Hospitalizations across the state continue to decline. As of Sept. 7, the Texas Department of State Health Services reported 3,537 people who are currently in the hospital for COVID-19, 666 fewer than seven days before. In addition, there are 2,057 new cases of COVID-19 in the state and a positivity rate of 7.2 percent.
The Houston Health Department announced additional testing sites for the week of Sept. 7.
Abbott extends disaster declaration
Gov. Greg Abbott extended the statewide disaster declaration on Monday for all Texas counties in response to the ongoing fight against COVID-19.
“Renewing this Disaster Declaration helps ensure that we have the resources and strategies in place to help communities across Texas respond to COVID-19,” Abbott said in a prepared statement. “I urge Texans to take precautionary steps to protect their health by wearing a mask, social distancing, and sanitizing their hands. Working together, we will slow the spread and keep our communities safe.”
Initially issued March 13, the disaster declaration allows Abbott to authorize the use of the state’s available and necessary resources to support COVID-19 efforts, as well as to reallocate resources in the state, including those obtained through the Strategic National Stockpile.
9 vaccine companies sign joint safety pledge
Today, the CEOs of nine biopharmaceutical companies signed a pledge of their commitment to seek approval or emergency use authorization from the U.S. Food and Drug Administration only for COVID-19 vaccines that are proven to be safe and effective.
AstraZeneca, BioNTech, GlaxoSmithKline, Johnson & Johnson, Merck, Moderna, Novavax, Pfizer and Sanofi signed a statement that read: “We, the undersigned biopharmaceutical companies, want to make clear our on-going (sic) commitment to developing and testing potential vaccines for COVID-19 in accordance with high ethical standards and sound scientific principles.”
Over the weekend, President Trump said during a White House news conference that a “very safe and very effective” vaccine could be available by October because of Operation Warp Speed. However, given the rigorous testing drugs must go through in order to ensure safety and efficacy, there are growing alarm about cutting corners during vaccine development.
Amid concerns of a rushed vaccine development process, the CEOs vowed to make safety their top priority in an effort to reinforce the public’s confidence in the ongoing pursuit of the first COVID-19 vaccine.
“With increasing public concerns about the processes that we are using to develop these vaccines and even more importantly the processes that will be used to evaluate the vaccines, we thought it was critical to come out and reiterate our commitment,” Pfizer CEO Albert Bourla said in an interview with Today.
The pledge comes a week after the Biotechnology Innovation Organization, a global biotech trade association, issued an open letter emphasizing that “public health, and the public’s trust in new medical products, are dependent upon the integrity, transparency and objective assessment of new data as they emerge.” — Shanley Pierce
UPDATE | September 4, 2020, 4 p.m.: As COVID-19 numbers in Texas continue to improve, experts raise concerns about a future surge in cases in the weeks following the upcoming Labor Day weekend, The Texas Tribune reports.
During an afternoon news conference, Mayor Sylvester Turner urged Houstonians to remain vigilant during the holiday.
“It’s important to remember the virus doesn’t take off because it’s an extended weekend or a holiday,” Turner said. “Please, please keep on your mask, engage in social distancing, proper hygiene—we don’t want to see the numbers go up two weeks from now because we decided to come together in big numbers over the Labor Day weekend.”
Turner also addressed recent national news coverage about COVID-19 related evictions in Harris County and reminded city and county residents to apply for the $60 million rental assistance program through the nonprofit BakerRipley. He reiterated that rental assistance remains available and there is no longer a deadline to apply, adding that any individual who wishes to contribute to the funding may contact BakerRipley directly.
Today, the Houston Health Department is reporting 510 new cases of COVID-19 and 13 additional deaths, bringing the city’s totals to 64,985 total cases and 862 deaths. The health department also shared a new video as part of its multilingual public health education campaign Better.Together. The agency encourages all residents to do their part to stop the pandemic by adopting behaviors that protect the community at large.
Notably, Houston Health Department-affiliated COVID-19 testing sites will be open on Saturday and Sunday this weekend, but the only city-run site open on Labor Day (Monday, Sept. 7) will be at Minute Maid Park.
The Centers for Disease Control and Prevention (CDC) told states to prepare to distribute a vaccine for COVID-19 by November 1. In a recent letter to governors, CDC Director Robert Redfield, M.D., wrote that “CDC urgently requests your assistance in expediting applications for these distribution facilities and, if necessary, asks that you consider waiving requirements that would prevent these facilities from becoming fully operational by November 1, 2020.” The news raises concern about political motives behind the push. Experts also urge caution on expediting a vaccine before thorough safety studies are complete.
According to the journal Nature, as of today there are 321 COVID-19 vaccine candidates worldwide; 32 have entered clinical trials.
STAT News recently reported on research surrounding individuals with sickle cell disease and their vulnerability to severe COVID-19 disease. The CDC has acknowledged that sickle cell disease is one of the many conditions that seems to put individuals at higher risk of severe illness if infected with the SARS-CoV-2 virus and the researchers are examining whether carrying just one copy of the sickle cell mutation could also influence the severity of a person’s COVID-19 disease.
A new study from The University of Texas Medical Branch at Galveston (UTMB) suggests that people with substance abuse disorders may also be at a higher risk of severe COVID-19 disease. Gathering data from more than 54,000 patients who tested positive for COVID-19 between February and June of this year, the researchers determined that individuals with substance abuse disorders died at higher rates and were more likely to be hospitalized and need ventilation.
The CDC also recently released a study that showed people across the U.S. complied with stay-at-home orders issued earlier this year. Researchers analyzed location data from cell phones and found that there was a measurable decrease in population movement in 97.6 percent of counties with mandatory stay-at-home orders.
Finally, two long-form pieces published this week are worth a read over the long weekend: a ProPublica investigation into some New Orleans hospitals that discontinued treatment and sent COVID-19 patients into hospice facilities or back home to die; and an essay by novelist Jesmyn Ward detailing the sudden death of her husband as COVID-19 was hitting the United States and her ensuing grief amid months of uncertainty and social unrest. — Alexandra Becker
UPDATE | September 3, 2020, 10 a.m.: The debate has started about the next phase of COVID-19 reopening in Texas as Labor Day weekend approaches.
Texas Gov. Greg Abbott hinted on Aug. 31 via Twitter about a forthcoming reopening process for the state that he plans to announce next week.
“I said last month that Texas wouldn’t have anymore (sic) lockdowns—despite demands from mayors & county judges insisting on lockdowns,” the social media message said. “Since my last orders in July, COVID (sic) numbers have declined—most importantly hospitalizations. I hope to provide updates next week about next steps.”
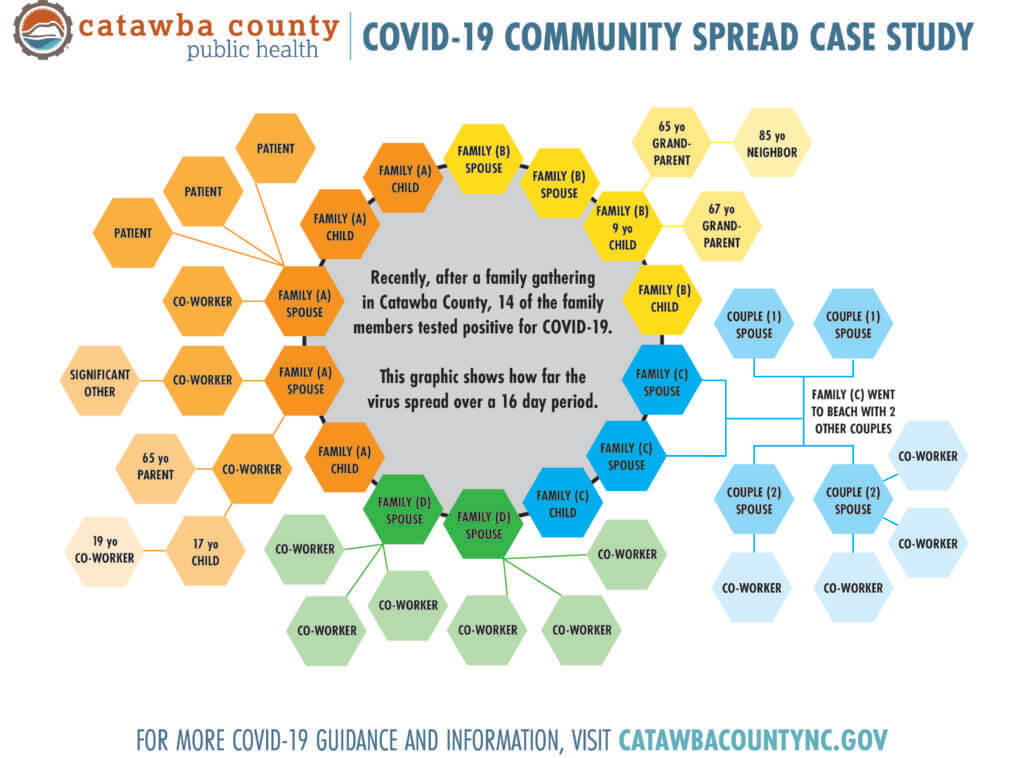
June increases in the city’s cases and hospitalizations were blamed on Memorial Day gatherings.
Houston Mayor Sylvester Turner, who leads the most-populated city in Texas, issued a lengthy response on Wednesday cautioning against reopening any time soon.
“We must remain vigilant and not reverse the hard work we have done to reduce COVID-19 positive cases and deaths. In March and April, cities and counties worked together with the media to slow the coronavirus progression. We were successful, and our numbers were better than those of most major cities around the country. Because the number of positive cases and deaths were low, the Governor commenced reopening businesses without consulting with local governments. In addition, he took away the authority from cities and counties to manage the response. The results were disastrous,” Turner wrote. “Thirty days later, the virus was out of control like a forest fire, and more people tested positive, more people died, and hospitals were scrambling to expand capacity. Consequently, the State ordered businesses to close for a second time, and Texas joined Florida, Arizona, and California in the national spotlight but not in the right way. In July, the Governor imposed a statewide mask requirement which was desperately needed, and he should be commended for that. … And now that numbers are better like in April, the Governor is about to embark on the same course again. It is frustrating that he is making decisions that impact all of us without including local officials in the process. The State is about to repeat its mistake, expecting a different result. Please tell that to the virus and explain that to the people who will suffer.”
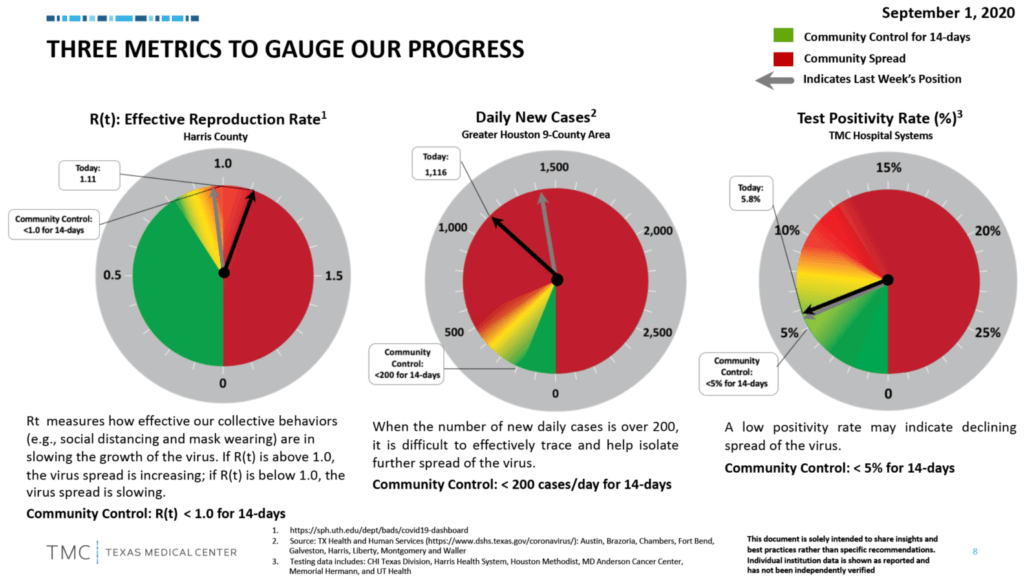
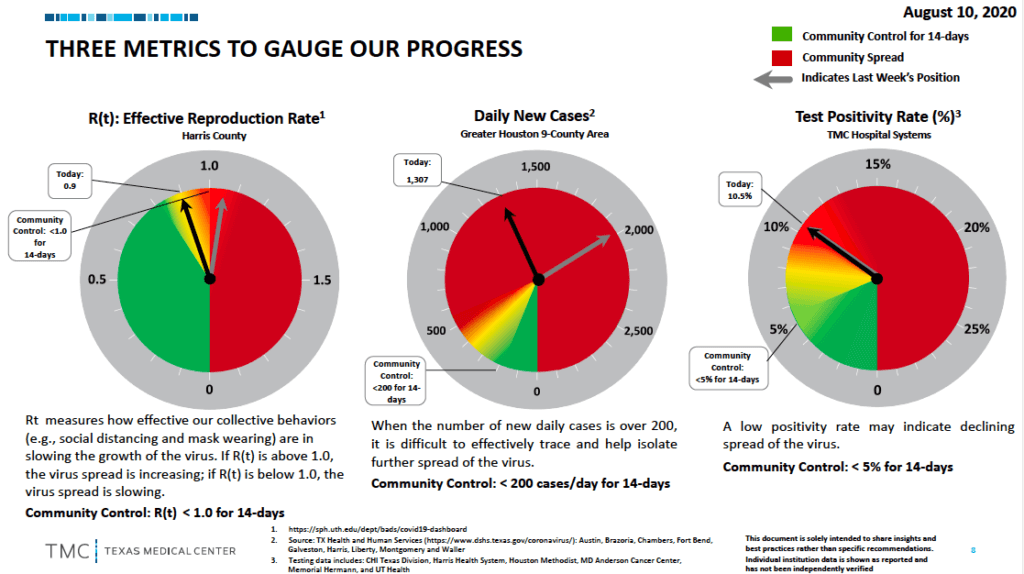
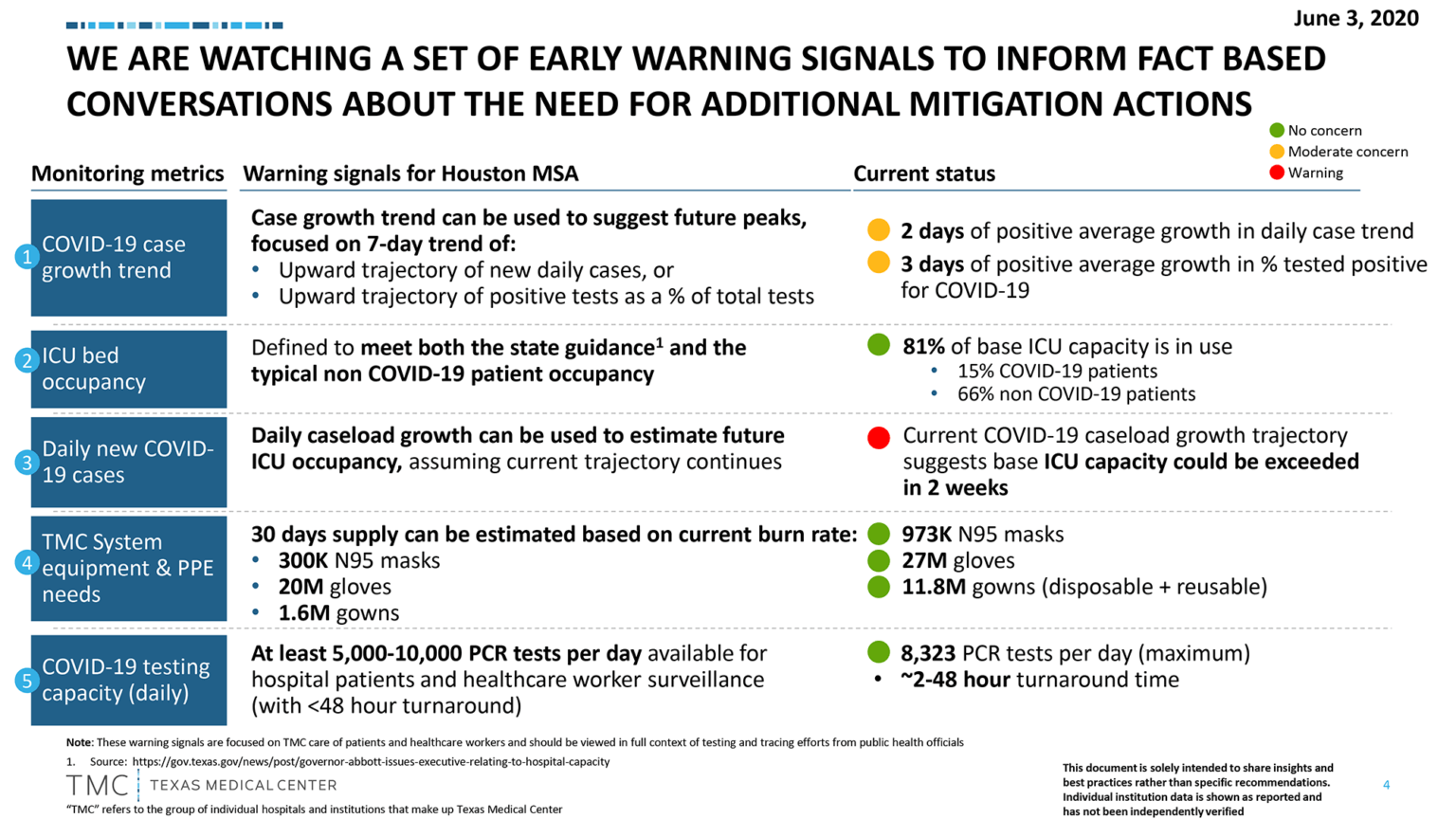
The Texas Medical Center, which also has advised caution, recommends following the progress of the area’s metrics on the effective reproduction rate, daily cases and the test positivity rate.
The aim is to land in the green zone. Here’s where we are now:
“Let’s get these metrics in the green. Our collective behaviors will help us isolate the further spread of this deadly virus. Don’t let the Labor Day holiday weekend hurt our progress and increase these rates,” the TMC Twitter account said on Sept. 2, continuing in a second Tweet. “As we start September and head into the #LaborDay weekend, remember that the #pandemic is not over. Together we can bring down the daily case growth and positivity rate. Be conscious of your actions, avoid large gatherings and always wear a mask to avoid the spread of #COVID19.” — Cindy George
UPDATE | September 2, 2020, 3:51 p.m.: The Houston Health Department is reporting 176 new cases and 18 new deaths, bringing the total to 64,137 cases and 841 deaths. The positivity rate is currently at 7.8 percent. While this is a significant improvement from a month ago when the high was at 23 percent, efforts to reduce the positivity rate to 5 percent or lower continue.
Houston to conduct antibody testing survey
On Wednesday, the Houston Health Department (HHD) announced a partnership with the Centers for Disease Control and Prevention (CDC), Rice University and Baylor College of Medicine to lead an antibody testing survey to determine the number of people who were previously exposed to SARS-CoV-2 and how the virus is behaving in the community.
HHD and Houston Fire Department paramedics will randomly select homes across the city to visit—asking households medical questions related to COVID-19 and collecting voluntary blood samples. Volunteers will receive antibody test results after approximately two weeks.
“If we knock on your door, I strongly encourage you and your loved ones to participate in this important survey,” Houston Mayor Sylvester Turner said in a prepared statement. “The data you provide by participating will help inform strategies to mitigate the effects of COVID-19.”
The citywide antibody testing survey will be implemented in two phases: The first phase will begin Sept. 8 through Sept. 24 and the second phase starting in January 2021.
WHO backs inexpensive corticosteroids for treatment of critically ill COVID-19 patients
Also on Wednesday, the World Health Organization published new guidance for the use of corticosteroids for patients with severe COVID-19.
The guidance is supported by new data, released Wednesday in the Journal of the American Medical Association (JAMA), collected from a meta-analysis of seven randomized trials with more than 1,700 patients. The results of the analysis confirmed that patients who were treated with one of the three corticosteroids— dexamethasone, hydrocortisone and methylprednisolone—had a lower mortality rate compared to those who received a placebo or usual care. Approximately 33 percent of patients treated with a steroid died, while 41 percent of patients who did not receive a steroid treatment died. The meta-analysis translated this into a 34 percent risk reduction of death thanks to steroids.
Of the three corticosteroids, dexamesthasone was the most effective, followed by hydrocortisone and methylprednisolone, respectively.
The WHO’s guidance, however, does not recommend using corticosteroids for patients with non-severe COVID-19 “given that current data indicated they would not likely derive benefit and may derive harm,” the organization wrote.
CDC halts evictions nationwide
The CDC issued a new temporary eviction ban across the country in an effort to prevent the further spread of COVID-19.
“Eviction moratoria facilitate self-isolation by people who become ill or who are at risk for severe illness from COVID-19 due to an underlying medical condition,” according to the order. “They also allow state and local authorities to more easily implement stay-at-home and social distancing directives to mitigate the community spread of COVID-19.”
The order, which is effective through the end of the year, also serves as a lifeline for people who have lost their jobs and otherwise have been affected negatively by the pandemic’s impact on the economy. — Shanley Pierce
UPDATE | September 1, 2020, 3 p.m.: The Houston Health Department is reporting today 127 new cases of COVID-19 and three new deaths from the virus, bringing the city’s totals to 63,961 cases and 823 deaths.
Yesterday, the U.S. surpassed 6 million reported COVID-19 cases.
Texas is among a group of states—including Arizona, California, Connecticut, Florida, Illinois, New Jersey and New York—disregarding the new national guidelines suggesting that testing asymptomatic individuals exposed to COVID-19 is not necessary. According to Reuters, a spokesman for the Texas Department of State Health Services reiterated that the state “recommends testing for all close contacts of a confirmed case because it allows for early case identification among people who are at a higher risk of infection.”
A “discussion draft” released today by The National Academies of Sciences, Engineering, and Medicine provides detailed recommendations about allocation of a COVID-19 vaccine once one becomes available. The report suggests the vaccine should first be provided to health care workers and adults with underlying medical conditions that put them at higher risk of severe COVID-19 disease. The National Academies released the discussion draft and is encouraging input from the public—especially from communities disproportionately affected by COVID-19—in order to finalize a report that is “objective, balanced, and inclusive.” The public comment period will close on Friday, September 4.
According to new data released by the Centers for Disease Control and Prevention (CDC), COVID-19 infections in health care workers treating COVID-19 patients may be higher than previously believed. The report examined 3,248 health care personnel from more than a dozen academic medical centers. Six percent of those individuals tested positive for SARS-CoV-2 antibodies, suggesting previous infection; 29 percent of those with antibodies were asymptomatic and 69 percent had not received a diagnosis. The study noted that the prevalence of SARS-CoV-2 antibodies were lower among health care workers who reported always wearing a face covering. The authors concluded that “a high proportion of SARS-CoV-2 infections among health care personnel appear to go undetected” and that “universal use of face coverings and lowering clinical thresholds for testing could be important strategies for reducing hospital transmission.”
A new national survey published by the journal Pediatrics explores COVID-19’s ongoing detriment to the well-being of parents and children in the U.S. Conducted in June, parents with children ages 18 and younger were asked about discernible changes in health status, insurance status, food security, use of public food assistance resources, child care and use of health care services since March 2020. The authors concluded that COVID-19 is having a substantial impact on both parents and children and suggested that policymakers “consider the unique needs of families with children, including support for mental and behavioral health and efforts to improve food security.”
Finally, an article in the journal Nature highlights challenges surrounding mortality statistics during the COVID-19 pandemic. The author, Giuliana Viglione, wrote that in times of upheaval such as wars, natural disasters or pandemics, researchers rely on measuring excess mortality—the comparison of expected deaths to those that occur—to rapidly tally deaths. She noted, however, that this metric has several flaws, including the fact that it does not distinguish between individuals who have died directly from the disease and those who died as a result of other factors related to COVID-19, including delayed routine care. It also relies on accurate and timely reporting, but “as with so many other aspects of the pandemic, the statistic has become politicized — a way for countries to claim superiority over one another,” Viglione added. — Alexandra Becker
UPDATE | August 31, 2020, 8 p.m.: First, the good news: Houston’s COVID-19 test positivity rate has been cut in half from 20% on July 31 to 7.8% on Aug. 27 and closer to the target of below 5%, according to the Houston Health Department.
PBS Newshour’s Monday evening broadcast featured the Texas Medical Center in the first report for a new series about the state of U.S. healthcare compared to the rest of the world. The story included pediatric cardiothoracic surgeon Jorge Salazar, M.D., of Children’s Memorial Hermann Hospital and UTHealth, and Elena Marks, J.D., MPH, CEO of the Episcopal Health Foundation and a health policy fellow at Rice University’s Baker Institute for Public Policy.
Houston firefighters are facing two colliding health emergencies, the COVID-19 pandemic and apparently escalating opioid addiction. Under a grant program called FRONTLINES, an acronym for First Responder Opioid Overdose Naloxone Training and Linkage into Needed Evidence-based treatment Services, emergency responders are able to administer Narcan, the nasal spray form of the lifesaving drug naloxone, “quickly and effectively,” according to a city news release. The drug restores normal breathing in people actively having a heroin or prescription opioid overdose. Naloxone is available by standing order across all pharmacies in the state of Texas without a separate prescription. Residents can legally possess and administer naloxone in Texas if they are personally at risk of opioid overdose or know someone who is.
For all of 2019, the Houston Fire Department used Narcan more than 1,300 times. So far in 2020, the drug has been used more than 1,000 instances.
“Now, more than ever, the entire Houston community needs to be aware that opioid misuse is a growing problem that could touch the lives of anyone including their own,” said David Persse, M.D., Houston health authority and the principal investigator of the FRONTLINES project. “Since people with opioid use disorder are disproportionately affected by the ongoing health and societal consequences associated with the COVID-19 pandemic, we all need to be ready to react quickly to save lives.”
The Houston Recovery Center, Baylor College of Medicine and the University of Texas at San Antonio are FRONTLINES grant partners.
“Rising unemployment and worsening mental health symptoms cause higher stress levels which may increase the abuse of substance like alcohol and illicit opioids, increasing the risk for opioid-related overdose,” the release said.
Harris County Public Health, with the Texas Health and Human Services Commission, is investigating multiple deaths and cases in what appears to be an ongoing COVID-19 outbreak at Heritage Park of Katy Nursing and Rehabilitation. The initial probe began in May after three people tested positive and the state began working with the facility. To date, there have been 14 deaths—four confirmed and 10 presumed—and another five people, residents and staff members, are being monitored currently for the virus.
Finally, on this last day of August, Houston is reporting eight new deaths attributed to COVID-19, bringing the city’s total to 820 as well as 158 new cases for a citywide continuing total of 63,834. — Cindy George
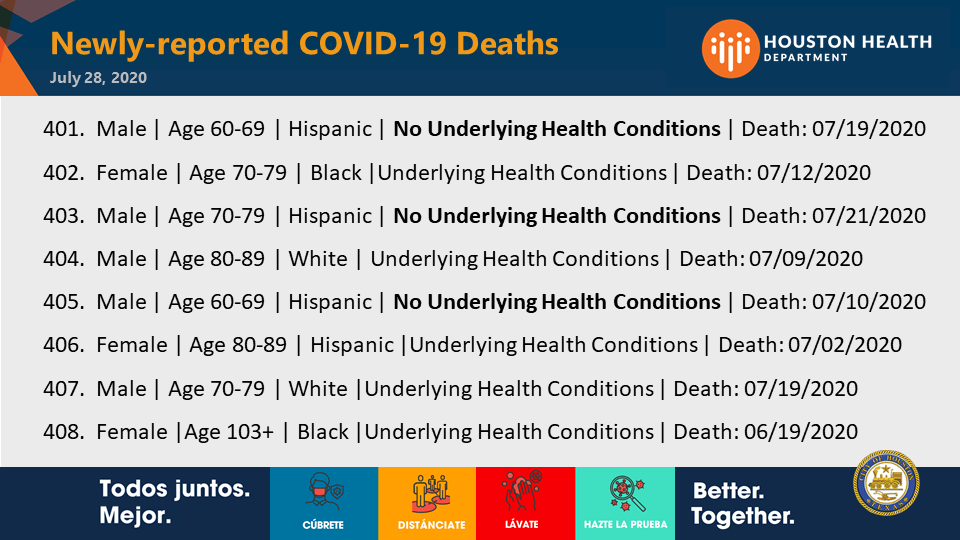
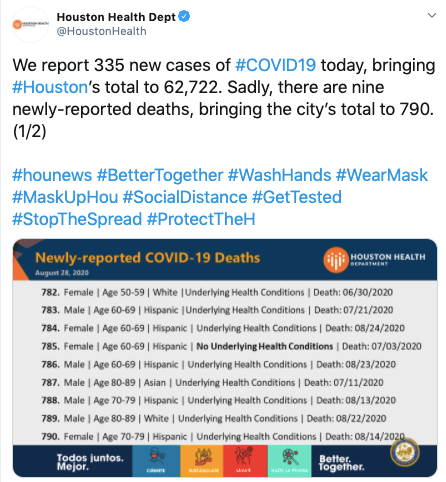
UPDATE | August 28, 2020, 3:45 p.m.: The Houston Health Department updated the latest COVID-19 numbers for the city this afternoon. There are 335 news cases today and nine new deaths, bringing the total number of deaths to 790.
Spread is slowing
Spread of the coronavirus is slowing in Harris County, according to Texas Medical Center data.
On Wednesday (Aug. 26), 1,370 people were reported as testing positive for COVID-19 in the Greater Houston Area, as compared to a week earlier, when 1,453 new cases were reported. One month earlier, 2,043 new cases were reported.
Also on Wednesday, 56 new COVID-19 patients were admitted to TMC hospitals, compared to 120 new COVID-19 patients admitted one week earlier. One month earlier, 197 patients were admitted.
Click here for the TMC’s daily Coronavirus (COVID-19) Updates.
COVID-19 Predictors
A study by researchers from the Harvard T.H. Chan School of Public Health showed that the biggest predictor of COVID-19 infection “was being a recent immigrant to the U.S., followed by living in a household with a large number of people and working in the food-service industry,” according to a report from STAT News.
While these three factors explained the high number of COVID-19 cases among Latinos, STAT reported, they did not explain high COVID-19 case rates among Blacks.
The study, which examined COVID-19 cases across Massachusetts cities and towns, “found that a 10 percentage point increase in the Black population was associated with a 312.3 increase in COVID-19 cases per 100,000, while a 10 percentage point increase in the Latino population was associated with an increase of 258.2 cases per 100,000.”
The study concluded that “independent predictors of higher COVID-19 rates included the proportion of foreign-born non-citizens living in a community, mean household size, and share of food service workers. After adjustment for these variables, the association between the Latino population and COVID-19 rates was attenuated. In contrast, the association between the Black population and COVID-19 rates persisted, and may be explained by other systemic inequities. Public health and policy efforts that improve care for foreign born non-citizens, address crowded housing, and protect food-service workers may help mitigate the spread of COVID-19 among minority communities.”
New education modules
The American Medical Association (AMA) this week announced a new series of open access educational modules that offer ways to support physicians during a time of acute stress.
Topics for the five new modules:
- Caring for the health care workforce in a crisis
- Establishing a Chief Wellness Officer position
- Providing a Chief Wellness Officer roadmap
- Providing peer support programs for physicians
- Optimizing patient portals
The modules are part of a collection available in the AMA STEPS Forward series, which is accessible through the AMA Ed Hub. — Maggie Galehouse
UPDATE | August 27, 2020, 3:20 p.m.: The Houston region was largely spared from Hurricane Laura last night, but the Category 4 storm caused widespread damage and power outages in Southeast Texas and Louisiana. COVID-19 testing sites affiliated with the Houston Health Department, which closed in anticipation of the weather event, will reopen tomorrow, Friday, August 28.
Today, the Houston Health Department is reporting 290 new cases of COVID-19 and 13 additional deaths, bringing the city’s totals to 62,387 cases and 781 deaths.
On Wednesday, the Centers for Disease Control and Prevention (CDC) proposed guidelines for future distribution of a COVID-19 vaccine in the U.S. once one is approved for public use. The guidelines were revealed during a presentation at the CDC’s Advisory Committee on Immunization Practices meeting. Among other recommendations, the CDC said they would prioritize health care professionals and essential personnel as well as seniors and individuals with underlying health conditions.
The U.S. Food and Drug Administration (FDA) granted emergency use authorization yesterday for the first rapid test for COVID-19 where results can be read directly from a testing card—similar to some pregnancy tests. The credit card-sized, self-contained test from Abbott Diagnostics will sell for $5 and shows results within 15 minutes.
“This new COVID-19 antigen test is an important addition to available tests because the results can be read in minutes, right off the testing card. This means people will know if they have the virus in almost real-time,” Jeff Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health, said in a statement from the FDA. “Due to its simpler design and the large number of tests the company anticipates making in the coming months, this new antigen test is an important advancement in our fight against the pandemic.”
The FDA also issued a warning today to consumers about hand sanitizers packaged in food and drink containers. In a statement, the agency noted that some hand sanitizers have been packaged in “beer cans, children’s food pouches, water bottles, juice bottles and vodka bottles” and that some even contain food flavoring, including chocolate flavoring. The FDA warned consumers about confusion as a result of the packaging, reiterating that any ingestion of these products can be toxic. The CDC issued a warning about ingesting hand sanitizer earlier this month.
Lastly, new federal guidelines regarding COVID-19 testing, which states that asymptomatic individuals do not necessarily need to be tested even if they have recently been exposed to a person with confirmed COVID-19 disease, continue to bring criticism. Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases, told CNN that he was in vocal cord surgery when the changes were discussed.
“I am concerned about the interpretation of these recommendations and worried it will give people the incorrect assumption that asymptomatic spread is not of great concern. In fact it is,” Fauci said in the CNN report. — Alexandra Becker
UPDATE | August 26, 2020, 2:35 p.m.: Hurricane Laura has been upgraded to a Category 4 storm with 140 miles per hour winds and is now moving east toward the Texas and Louisiana border. It is expected to make landfall from Wednesday evening to early Thursday.
Obesity increases risk of COVID-19 death by nearly 50 percent
A new study showed that obesity plays a significant role in how COVID-19 affects people who are overweight.
A team of researchers from the University of North Carolina at Chapel Hill reviewed published literature and immunological data of 399,461 diagnosed patients from other studies to determine the mechanisms behind the epidemiological relationship between obesity and COVID-19. They discovered that people who had a body mass index over 30 were 113 percent more likely to be hospitalized, 74 percent more likely to be admitted to the intensive care unit and 48 percent higher risk of death from SARS-CoV-2.
Early on, health experts were aware that obesity was among the various underlying risk factors for severe COVID-19, such as hypertension, heart disease and diabetes.
Obesity can trigger a chain of metabolic changes in the body, including insulin resistance and inflammation, that makes the body more susceptible to infection and uncontrolled serum glucose. This can, ultimately, disrupt the proper functioning of immune cells and impair the body’s ability to fight off SARS-CoV-2 and other pathogens.
In addition, these factors will also play a role in how effective vaccines are in people with obesity. Because obesity weakens the body’s immune response, researchers are concerned that future COVID-19 vaccines will not be as effective for those who are overweight.
The 6-foot distancing rule is outdated, report says
Maintaining a distance of at least six feet is standard in current safety guidelines to reduce the risk of community spread of COVID-19. However, researchers from the Massachusetts Institute of Technology and University of Oxford recently published a report that said the rule is outdated and an oversimplification.
“Rules that stipulate a single specific physical distance (1 or 2 metres) between individuals to reduce transmission of SARS-CoV-2, the virus causing covid-19, are based on an outdated, dichotomous notion of respiratory droplet size,” the researchers wrote in their report, published in the BMJ. “This overlooks the physics of respiratory emissions, where droplets of all sizes are trapped and moved by the exhaled moist and hot turbulent gas cloud that keeps them concentrated as it carries them over metres in a few seconds.”
The authors of the report said that force of emission from activities such as coughing and shouting can produce aerosol particles that can travel through the air more than six feet. In addition, other factors—including crowd size, ventilation and exposure time—also need to be taken into consideration to provide greater protection in high-risk settings.
They developed a color-coded chart that factored in the different variables—indoor or outdoor setting, crowd size, exposure time, ventilation and volume level (silent, speaking shouting/singing)—to determine risk.
CDC changes testing guidelines
Some asymptomatic people may not need to be tested for COVID-19, according to the Centers for Disease Control and Prevention’s updated testing guidelines.
Previously, the CDC encouraged people who were recently in close contact with an infected person or suspected being exposed to get tested, with or without symptoms.
According to the CDC’s website on July 17: “Testing is recommended for all close contact of persons with SARS-CoV-2 infection.” The agency emphasized that, due to the potential for asymptomatic and pre-symptomatic transmission, “it is important that contacts of individuals with SARS-CoV-2 infection be quickly identified and tested.”
However, in an about-face, the CDC updated its page on Aug. 24. It now states that, even if you were potentially exposed to COVID-19 but are not symptomatic, you might not need a test: “If you have been in close contact (within 6 feet) of a person with a COVID-19 infection for at least 15 minutes but do not have symptoms: You do not necessarily need a test unless you are a vulnerable individual or your health care provider or state or local public health officials recommend you take one.” — Shanley Pierce
UPDATE | August 25, 2020, 2 p.m.: Three years ago today, Hurricane Harvey made landfall in Houston. Now, all eyes are on Hurricane Laura, which is currently expected to make landfall as a Category 3 storm late Wednesday evening and into Thursday morning. The City of Galveston has issued a mandatory evacuation for all residents on the island and Harris County Judge Lina Hidalgo has requested a voluntary evacuation for all residents living in zones A and B in Harris County, which are along the coast.
During a midday news conference, Hidalgo urged all residents to be prepared for high winds and power outages as a result of the storm.
“Let me make this as clear as possible: All of us need to be prepared for the very real potential of a direct hit from this storm,” Hidalgo said. “This is truly when we have to say: ‘Prepare for the worst.’”
Hidalgo said that evacuees should remember to bring COVID-19 essential items, including masks and hand sanitizer. She also asked inland residents to stay off the roads as much as possible to make room for those evacuating the coast, but reiterated that every person in Harris County should make preparations to shelter in place.
Mayor Sylvester Turner joined Hidalgo at the news conference, adding that he expects residents to be at home and off the roads by 8 p.m. tomorrow as high winds are anticipated by then.
“The tracking of this storm has been somewhat unpredictable, but what is consistent is that this is a dangerous storm,” Turner said. “It has gone from a Category 2 to now a Category 3, and who knows where it may end up? So, I do want to emphasize people taking this storm seriously.”
Updates and guidance about preparation are available at ReadyHarris.og.
In COVID-19 news, Houston’s positivity rate yesterday fell to 9.2 percent, the lowest since May.
The Texas Tribune also reported that COVID-19 hospitalizations have dropped by a quarter in the last week. Because of the anticipated weather, COVID-19 testing sites affiliated with the Houston Health Department will be closed tomorrow, August 26, and on Thursday, August 27.
For the most up-to-date data on COVID-19 infections in the Houston area, visit the COVID-19 dashboard maintained by Harris County Public Health and the Houston Health Department.
Researchers in Hong Kong have identified an individual who was re-infected with a different variant of COVID-19. The 33-year-old male first contracted the virus in March, had fully recovered and then contracted it again nearly five months later. He was asymptomatic after the second infection, possibly indicating that the first infection did provide some immunity.
A new study published yesterday in JAMA found that internet searches related to acute anxiety shot up by 11 percent between March 13, 2020 and May 9, 2020, the two months after President Trump declared COVID-19 a national emergency. The authors of the study said the spike—which translated to a total of 3.4 million searches—was an all-time high for searches related to acute anxiety and panic attacks. The largest spike in anxiety queries occurred on March 28, 2020, with a 52 percent increase.
Finally, Baylor College of Medicine has begun recruiting for a nationwide study to observe COVID-19 in patients with cancer. The study, conducted by the National Cancer Institute, aims to understand risk factors for developing a severe case of COVID-19 in individuals who are receiving cancer treatment and how COVID-19 may impact the course of cancer treatment and patient outcomes. Individuals interested in joining the study should email Claire.hoppenot@bcm.edu. — Alexandra Becker
UPDATE | August 24, 2020, 3:30 p.m.: Houston now faces the “double crisis” of a hurricane threat and COVID-19, as the situation was described today by Harris County Judge Lina Hidalgo during a news conference with Houston Mayor Sylvester Turner and emergency management officials.
Laura is now predicted to make landfall as a Category 2 hurricane late Wednesday or early Thursday near the Texas-Louisiana border, according to the National Hurricane Center. Tropical Storm Marco, closer to the Gulf Coast, has fizzled.
“Thankfully, any substantial threats from Marco to our region have receded. We expect its coming ashore will have minimal impacts in our area—maybe some light showers and thunderstorms,” Hidalgo said. “We must now focus on Laura. Laura is expected to strengthen to a hurricane tomorrow, making landfall very early Thursday morning somewhere between Freeport, Texas, south of Houston, and Lake Charles, Louisiana. Depending on where it goes, it could have minimal impact in our region or it could have very significant storm surge.”
The public should know that the Red Cross has been preparing for socially distanced sheltering, Hidalgo said.
“The Red Cross is prepared to open emergency shelters. If sheltering is required, folks should not fear visiting those shelters,” the county judge said. “They have worked with FEMA, with the CDC, to take all precautions related to COVID-19.”
Visit ReadyHarris.org for storm updates and to register for Ready Harris Alerts.
Hidalgo urged people to prepare now as there is a short window.
“Make sure you have a full tank of gas, that you have supplies for your home, including medications, PPE, face coverings, hand sanitizer. Think about what you may need if there were prolonged power outages. Don’t forget about your pets,” Hidalgo said. “For folks living along the coast: Listen to your local elected officials about if and when to evacuate, should that become necessary. We won’t have a clear forecast until probably tomorrow morning, so the turnaround will be very quick. Anyone along the coast should prepare as if you were going to be asked to evacuate. You should be ready to go at a moment’s notice.
As the three-year anniversary of Hurricane Harvey approaches, Turner called our area “battled-tested” and ready for an expected wind event.
“We do not anticipate this storm to stall,” he said. “This is not Harvey. This is not anticipated to be a heavy rain event.”
On a more upbeat note, the COVID-19 positivity rate in Houston has dipped under 10% and closer to the target of below 5%, according to the Houston Health Department. — Cindy George
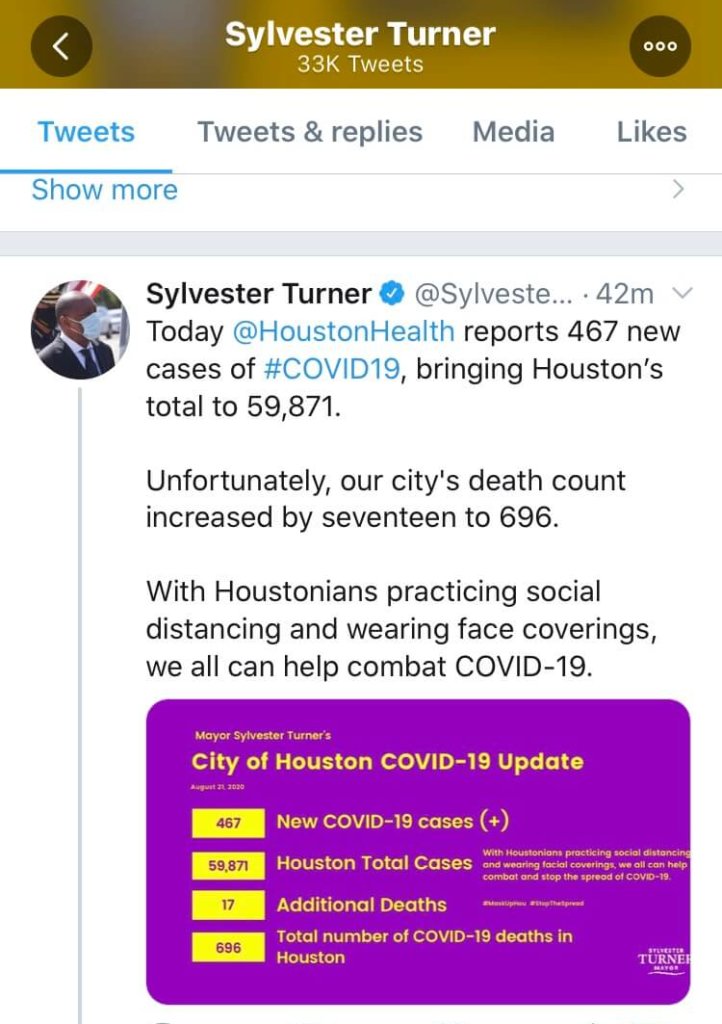
UPDATE | August 21, 2020, 4 p.m.: Houston Mayor Sylvester Turner today captured the city’s latest COVID-19 numbers in a tweet:
In an afternoon press conference with local leaders, Turner said Houstonians should be “weather-alert and prepared” as two tropical storms make their way to the Gulf Coast over the next few days.
Approaching storms do not change the reality of COVID-19, he added.
“As the storms come, the virus does not take a break,” Turner said. “Let me encourage you, for example, instead of waiting for Monday or Tuesday to get tested, go today, go tomorrow, go Sunday. … The testing site at Minute Maid Park is open seven days a week.”
Should the storms bring flooding and individuals become displaced, those individuals will need to know their COVID-19 status.
“If you end up having to, let’s say, shelter at home or bunk with family members and friends, or potentially go to a shelter, you really need to know your COVID status,” Turner said. “So please get tested. … If you don’t do it for yourself, do it for the first responders.”
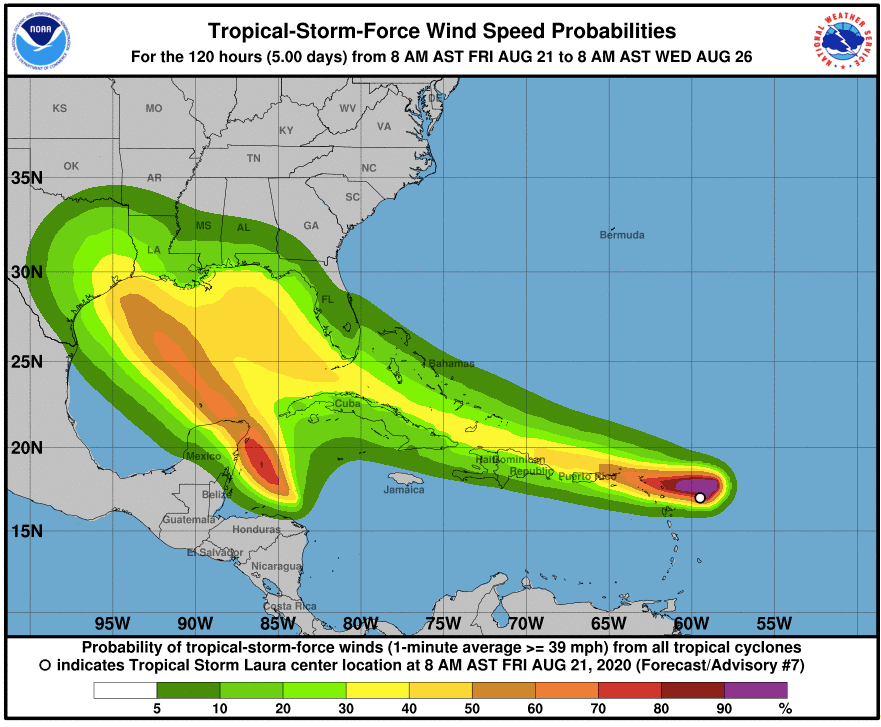
This National Weather Service chart shows expected activity along the Texas Gulf Coast over the next few days.
Houston Fire Chief Samuel Peña cautioned Houstonians not to drive through flooding or flooded streets.
“It doesn’t take but 18 inches of water for your car to be swept away,” Peña said.
In the event of a power outage, remember the regular supplies—including flashlights, batteries, water—as well as masks and sanitizer, he added. And make provisions for pets.
“Keep your cell phones charged,” Peña said. “If there’s a degradation of cell phone service, remember that texts a lot of times will go through when calls will not.”
David Persse, M.D., Houston’s health authority, reminded the public that hospitals never serve as shelters in the event of flooding, and that remains true in the time of a pandemic.
“Be thinking ahead,” Persse said. “Hospitals are safe places to go if you need to be there, but they are not to be used as shelters.” — Maggie Galehouse
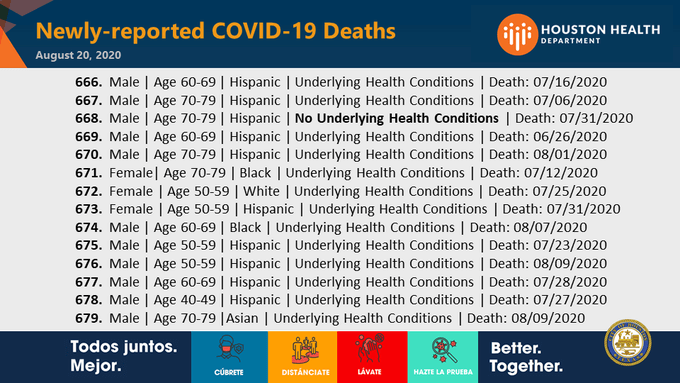
UPDATE | August 20, 2020, 8 p.m.: The City of Houston sadly reports 14 new COVID-19 deaths, bringing the total to 679. The city reported 501 new cases on Thursday for a tally of 59,404 so far during the pandemic.
The Asia Society Texas Center will host a webcast entitled “New Realities and Challenges: Coronavirus in the Fall” with Marc Boom, M.D., president and CEO of Houston Methodist, about the current state of the pandemic, our response and what’s next.
The program, to be streamed live on YouTube and Facebook, will begin at 7:30 p.m. Thursday, Sept. 10. Click here for links to the live event and to receive a reminder email about the program.
Former Secretary of State James Baker III and his wife, Susan, have been diagnosed with COVID-19 and are quarantined in their Houston home. According to Baker’s spokesman, the couple was likely exposed to the virus while visiting relatives last week in Wyoming. The 90-year-old Baker, a Houston native, served under three presidents: secretary of state under President George H.W. Bush, secretary of the treasury for President Ronald Reagan and undersecretary of commerce for President Gerald Ford. — Cindy George
UPDATE | AUGUST 19, 2020, 3:45 p.m.: The Houston Health Department is reporting 349 new cases of COVID-19 and 10 additional deaths today, bringing the city’s totals to 58,903 cases and 665 deaths.
During an afternoon press conference, Mayor Sylvester Turner encouraged everyone in the area to get tested because of the high rate of asymptomatic individuals. Houston health authority David Persse, M.D., also spoke during the press conference, stating that the city’s ability to accurately measure positivity rate is dependent on people getting tested. Persse also cleared up confusion about an increase in the city’s positivity rate, explaining that it was due to a large backlog of positive test results from the state after an upgrade to its computer system allowed the processing of more test results more quickly. Notably, positive tests are prioritized. Persse said the city is still anticipating a large number of negative test results from the same time period. The situation at hospitals continues to improve and that the percentage of patients in the ICU is steadily declining, Persse added.
On Tuesday, the Texas Medical Center admitted 123 new COVID-19 patients in TMC hospital institutions and the current seven-day average COVID-19 testing positivity rate is 8.6 percent. The TMC is also reporting an effective reproduction rate below 1.0 for the ninth day in a row at .79, which indicates that the virus spread is slowing.
Harris County Public Health (HCPH) issued a statement yesterday regarding a joint letter sent from several Houston-area public school districts in response to the health authority’s Harris County Schools Reopening Roadmap. The new statement makes clear that current indicators are not safe for resuming in-person school activities in Harris County and recommends that in-person activities be phased in until community spread of COVID-19 declines:
“To monitor and inform phased-in approaches for in-person activities, HCPH has recommended a set of benchmarks and metrics to monitor for public health trends. These indicators do not mean that in-person activities for schools will be closed indefinitely until a vaccine is available and the pandemic is over. Rather it is up to all of us to assure that our schools can go back to in-person learning sooner than later,” the statement read.
Meanwhile, UT Physicians is currently offering a corporate COVID-19 testing program to help organizations to safely bring employees back to the office. The program provides on-site testing and offers a discounted rate for larger organizations; results are usually available in two to three days.
A new survey conducted by The Physicians Foundation has found that the majority of doctors do not believe COVID-19 will be under control before January 2021 and that nearly half do not see the virus being under control until after June 2021. The majority of the physicians surveyed also expressed that the pandemic will likely severely impact patient health outcomes due to delayed routine care.
And, according to The New York Times, there have now been more than 1,000 COVID-19 related deaths among prison inmates and correctional officers.
STAT News is exploring a lack of data for pregnant women and children as drug developers work toward creating a COVID-19 vaccine.
“Manufacturers that are testing the vaccines in clinical trials have so far not included pregnant women or women who are breastfeeding. And only one of the vaccine makers that may end up supplying the American market, AstraZeneca, has started to test its vaccine in children,” the story’s author, Helen Branswell, wrote.
Finally, news broke this morning that the U.S. Food and Drug Administration (FDA) has temporarily halted its emergency use authorization for blood plasma as a treatment for COVID-19 over concerns about sufficient data. The New York Times reported that H. Clifford Lane, M.D., deputy director for clinical research and special projects at the National Institute of Allergy and Infectious Diseases, said that an emergency approval still could be issued by the FDA in the near future after more data is reviewed. — Alexandra Becker
UPDATE | AUGUST 18, 2020, 2 p.m.: On Monday, Texas became the fourth state to exceed 10,000 COVID-19 deaths, joining California, New Jersey and New York in the milestone death toll.
The positivity rate statewide is declining and is currently at 11.8 percent—a significant drop from last week’s rate of 24.5 percent, which state health officials attributed to backlogs, coding errors and a system upgrade in the laboratories conducting the tests.
The positivity rate across Texas Medical Center hospital systems and Harris County is 8.6 percent and 13.4 percent, respectively.
WHO issues letter calling for global COVID-19 vaccine pact
As the World Health Organization’s Aug. 31 deadline to join a global alliance for COVID-19 vaccines nears, WHO Director-General Tedros Adhanom Ghebreyesus urged its 194 members to prevent “vaccine nationalism” by participating in a joint effort to share vaccines with developing countries. He issued a letter today encouraging more countries to support equitable access to COVID-19 vaccines.
The COVAX Global Vaccines Facility pools resources and agrees to share limited supplies of medicines and vaccines to help countries around the world fight COVID-19. Currently, 92 underdeveloped countries and 80 wealthier nations—not including the United States—have signed on to participate in COVAX.
“Sharing finite supplies strategically and globally is actually in each country’s national interest,” Tedros said Tuesday during a virtual briefing. “No one is safe until everyone is safe.”
In June, the U.S. secured virtually the entire world supply of remdesivir, purchasing 500,000 doses of the potentially lifesaving drug. Through an agreement between Gilead Sciences and the U.S. Department of Health and Human Services, the nation was able to procure 100 percent of Gilead’s July production and 90 percent of its August and September supplies, raising concerns about how other countries would be able to receive their fair shares of the drug.
Gilead announced earlier this month that it will be able to make enough remdesivir to meet the global demand in October, with plans to produce more than 2 million treatment courses of remdesivir by the end of 2020 and “several million more in 2021, if needed.”
But if countries continue with the approach of vaccine nationalism, it will prolong the COVID-19 pandemic. Instead, an equitable global strategy to the allocation of lifesaving medicines and vaccines is the best approach to reduce transmission of COVID-19 worldwide.
Tedros proposed rolling out the allocation of vaccines in two phases. The first will proportionately distribute vaccines to all participating countries at the same time to reduce overall risk. Allocating vaccines for 20 percent of the population would cover most at-risk groups, such as adults 65 of age and older with underlying health conditions, in the majority of countries, Tedros said. In the second phase, more vulnerable countries facing higher threats of COVID-19 will be prioritized.
There are currently more than 165 candidate vaccines being developed around the world, with 31 in in-human trials and two approved for early or limited use.
“Like an orchestra, we need all instruments to be played in harmony to create music that everyone enjoys,” Tedros said. “One or two instruments playing by themselves just won’t suffice when the world is waiting and listening intently. We will work to bring the band together, to promote science, solutions and solidarity because we believe to our core that we do it best, when we do it together.”
New study shows no association between hospital visits and SARS-CoV-2 infection
Throughout the COVID-19 pandemic, patients have avoided visiting hospitals to seek medical attention out of fear of SARS-CoV-2 infection in the health care setting. However, a new study published in The Journal of the American Medical Association showed that there was “no meaningful association” between visits and rate of infection.
Because obstetrical patients require frequent visits to the hospital, scientists from Mass General Brigham in Boston decided they were a unique group that could help determine whether or not in-person health care visits were associated with SARS-CoV-2 infection. The team studied obstetrical patients who were tested for SARS-CoV-2 upon admission from April 19 to June 27. Of the 2,968 deliveries, 111 patients tested positive—45 before giving birth and 66 at the time of labor and delivery.
“The findings from this obstetrical population who had frequent in-person visits … suggest in-person health care visits were not likely to be an important risk factor for infection and that necessary, in-person care can be safely performed,” the authors wrote. — Shanley Pierce
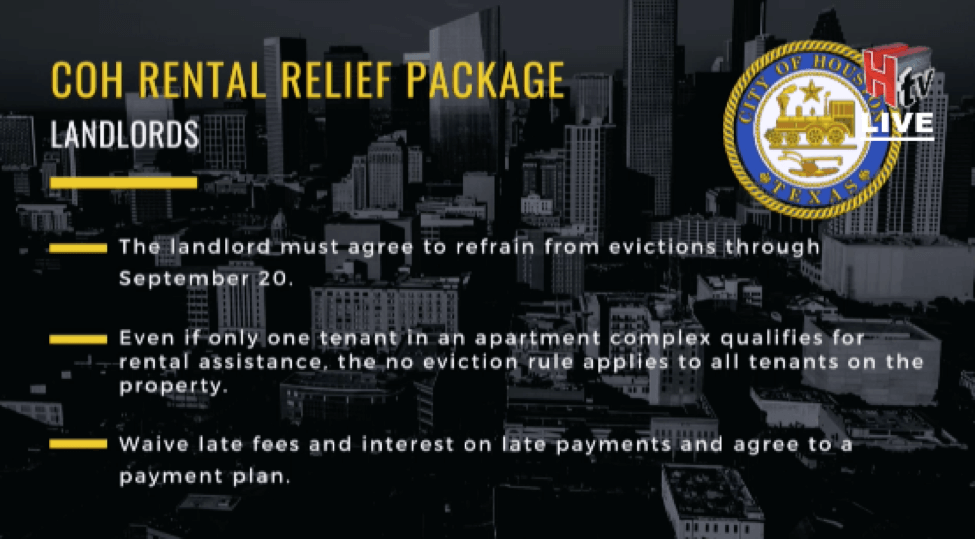
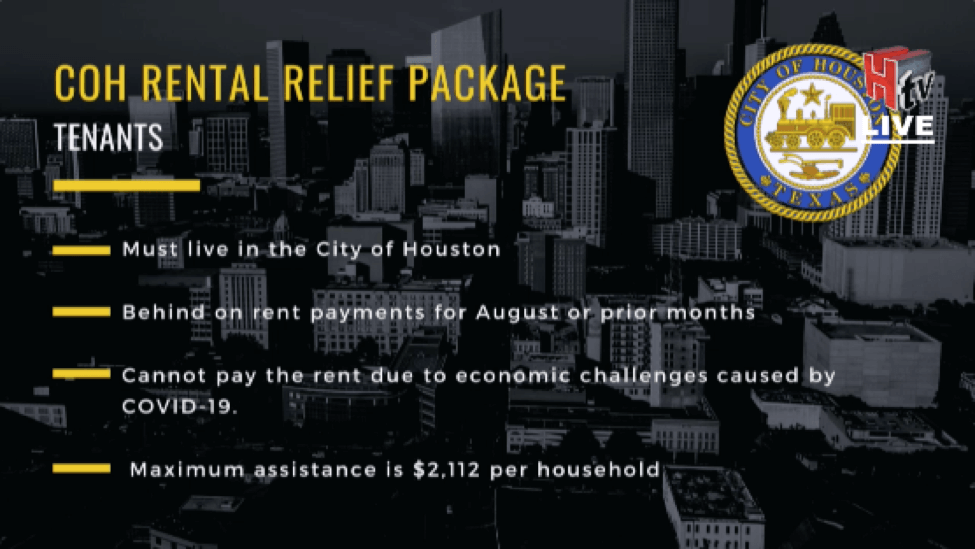
UPDATE | August 17, 2020, 4 p.m.: Houston Mayor Sylvester Turner today announced details about rental assistance for local residents and economic relief for small businesses affected by COVID-19.
Today through Aug. 26, landlords can enroll in the COVID-19 Rental Assistance Program administered by BakerRipley. To qualify, landlords must have units inside the City of Houston; landlords must agree to waive all late fees and interest; landlords must refrain from evictions through September 2020; landlords must enter into a payment plan with their tenants through Nov. 1; and landlords must rescind any prior eviction processes, Turner said.
Houston Mayor Sylvester Turner discusses rental assistance and small business relief programs at an Aug. 17, 2020 news conference.
Starting next week, from Aug. 24 through Aug. 30, tenants can apply to receive up to $2,112 for delinquent rent for August or prior months, so long as their landlords are participating in the city’s COVID-19 Rental Assistance Program. When a tenant is selected and qualifies for the program, his or her landlord will be paid directly by BakerRipley.
Small businesses also will be eligible for financial assistance beginning Aug. 19, when applications open for the City of Houston’s Small Business Economic Relief Program. Applications will close on Sept. 4.
“This is a $15 million relief grant program which is funded through the federal CARES Act,” Turner said. “It will help small businesses in our city who have been adversely impacted by the COVID-19 pandemic.”
Go to cityofhouston-sberp.org to submit an application.
The mayor also updated the city’s COVID-19 numbers, reporting 354 new cases, which brings the total number of cases to 58,172. Total deaths in the city so far are 649.
New saliva test for COVID-19
“The method, called SalivaDirect, is being further validated as a test for asymptomatic individuals through a program that tests players and staff from the National Basketball Association (NBA),” according to information released by YaleNews. “SalivaDirect is simpler, less expensive, and less invasive than the traditional method for such testing, known as nasopharyngeal (NP) swabbing. Results so far have found that SalivaDirect is highly sensitive and yields similar outcomes as NP swabbing.”
Yale gave the saliva test to a group including NBA players and staff “in the lead-up to the league’s return to play and compared results to the nasal swab tests the same group took,” said a report from ESPN. “The results almost universally matched, according to published research that has not yet been peer-reviewed.”
Researchers are not looking to commercialize the method. Rather, they hope the test will help those most in need.
The testing method works with reagents and instruments that are available from multiple vendors, which means that supply chain issues with certain vendors won’t stymie testing altogether. Researchers said the testing method is available now to diagnostic labs that want to start using the new test, which can be scaled up for use across the nation and beyond in the coming weeks.
Free COVID-19 testing
The Houston Health Department is offering free COVID-19 tests this week at two sites: Darrell Tully Stadium at 1050 Dairy Ashford; and Kingwood Park Community Center at 4102 Rustic Woods Drive. Each site, open from 10 a.m. to 7 p.m. today through Aug. 22, offers 1,250 tests daily. For an appointment, go to doineedacovid19test.com or register on site.
The department also offers free drive-thru testing at Delmar Stadium and Butler Stadium. Each site is open Monday to Saturday from 8 a.m. to 3 p.m. or until reaching daily capacity of 650 tests.
Recently, the sites have been testing about 250 people a day, according to Houston health authority David Persse, M.D., so there is plenty of testing availability. Those who would like to get tested at Delmar Stadium, 2020 Mangum Rd., should call 832-393-4220 between 7 a.m. and 4 p.m. to receive an access code. Butler Stadium, 13755 S. Main St., no longer requires an access code. — Maggie Galehouse
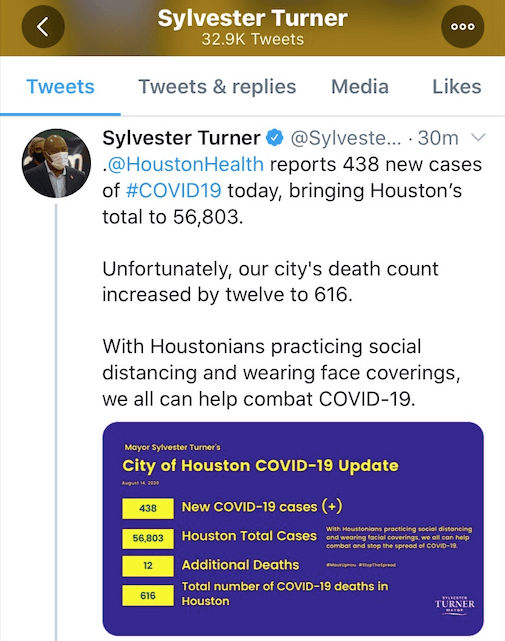
UPDATE | August 14, 2020, 4 p.m.: An afternoon tweet from Houston Mayor Sylvester Turner updated the city’s COVID-19 numbers:
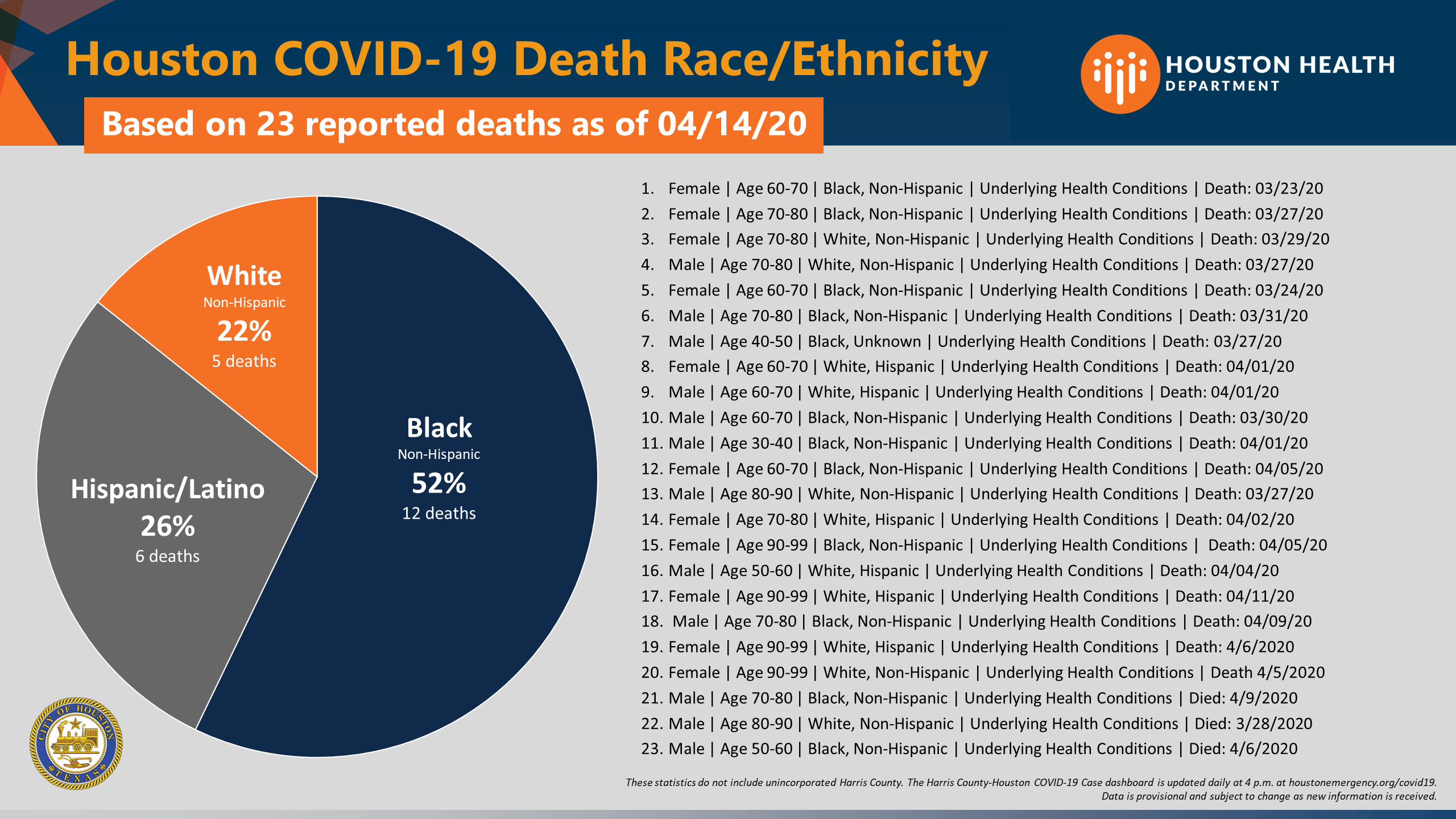
The racial breakdown of the 12 new deaths follows trends the city has already reported: five individuals were Black, four Hispanic, two white and one Asian.
COVID and Census 2020
A joint statement from the U.S. Census Bureau and the Centers for Disease Control and Prevention (CDC) this week spoke to in-person follow-up interviews with households that have not responded to Census 2020.
Census takers must abide by the following CDC recommendations to mitigate the risk of transmission of COVID-19:
- Wearing of face masks
- Maintaining social distance of 6 feet or more
- Practicing hand hygiene
- Not entering homes, and conducting interviews outside as much as possible or practical
Household members encountered by census staff should maintain appropriate social distance during interviews and practice the other recommendations on the CDC’s list as much as possible.
So far, an estimated 60 percent of households in the U.S. have responded to the 2020 Census. A complete count ensures every household, city, county and state receives its fair share and avoids a decade-long loss of resources and representation. The census impacts access to health care, housing, education, transportation and nutritional assistance—all elements of public health.
The FDA’s role in containing the pandemic
American Medical Association President Susan R. Bailey, M.D., spoke with U.S. Food and Drug Administration Commissioner Stephen M. Hahn, M.D., about the FDA’s role in containing the pandemic. Their conversation took place during a videoconference in partnership with the Reagan-Udall Foundation.
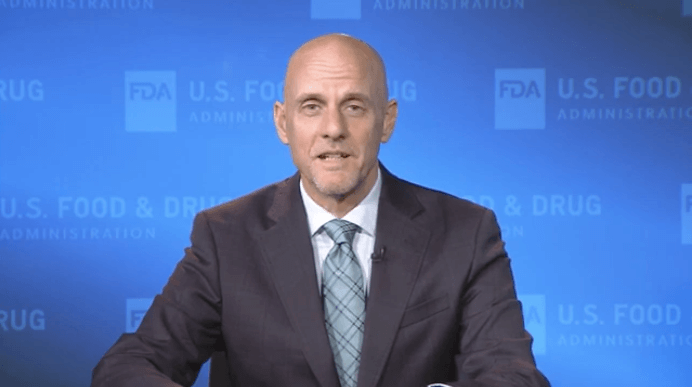
FDA Commissioner Stephen M. Hahn, M.D., spoke with American Medical Association President Susan R. Bailey, M.D., about COVID-19.
With regard to the urgency to develop and approve new tests, therapeutics and vaccines for COVID-19, Hahn said: “Let me assure you, we will not cut corners. All of our decisions will be based on good science.”
Doctors are learning more every day about COVID-19, added Hahn, who served as chief medical executive at The University of Texas MD Anderson Cancer Center before his confirmation as FDA commissioner in December 2019.
“We’re all concerned about the reports of rising case counts in different locations across the U.S., particularly in the Sun Belt states,” he said. “The emerging data also continue to confirm the disproportionate impact of the disease on different communities based on age, ethnicity and race. And as health care providers, this must be top of mind for us.”
The FDA is asking for clinical endpoints, rather than immunological endpoints, from the vaccine trials, Hahn added.
“We don’t have a complete data set showing that the development of antibodies is yet protective of someone from getting reinfection,” he said. “Now, that may emerge over the next several months and that would be great. But in the absence of those data, we can’t use the immunologic response, either the antibody or a T cell response to a vaccine as a surrogate for prevention. So we’ve insisted upon the fact that what we want to see is this 50 percent reduction in either prevention of someone getting COVID-19 who’s been exposed, or in converting COVID-19 to a very benign disease, something like the common cold.” — Maggie Galehouse
UPDATE | August 13, 2020, 8 p.m.: COVID-19 public health risks are being addressed at Houston’s homeless encampments with a new deep-cleaning effort. On Thursday, Mayor Sylvester Turner observed crews sweep debris and remove furniture from a freeway underpass at Bellfort and the Gulf Freeway (I-45).
Crews complete sanitation by disinfection and pressure washing before homeless services counselors assist houseless individuals. Turner was joined by city Solid Waste Director Harry Hayes, Council Member Robert Gallegos and Marc Eichenbaum, director of the mayor’s homeless initiatives.
Since April, Solid Waste has worked with council members and community groups on weekly debris removal at 70 sites across the city to prevent the communal spread of COVID-19.
In June, the Houston City Council approved the purchase of special COVID-19 cleaning units, including six pickup truck-trailer combinations and two rear loaders for heavy materials.
Eichenbaum said the cleanup is part of the city’s COVID-19 response along with counseling for homeless people.
“We have to make sure, per CDC guidelines, that the sanitation improves in encampments and in places where homeless individuals are residing and that we can get them permanently out of here with housing,” Eichenbaum said.
During the pandemic, the city announced a $65 million partnership with Harris County to provide permanent, supportive housing to 5,000 people over the next two years.
On Thursday, Houston reported 19 new deaths, bringing the city’s total to 604, as well as 425 new cases for a cumulative sum of 56,365. Click here for the Harris County/Houston combined COVID-19 dashboard.
This week, The New York Times published Inside the Fight to Save Houston’s Most Vulnerable, a multimedia look from the front line of a COVID-19 intensive care unit at Houston Methodist Hospital. The storytelling emphasizes that most of the patients on the unit were Latino, a population hit hard by COVID-19 infections and hospitalizations and disproportionate deaths. The five Latino patients profiled come from high-risk groups including essential workers, those with underlying conditions and a transplant recipient.
The Houston Health Department is now offering in-home COVID-19 testing for the homebound who are 60 and older, persons with disabilities and veterans. For more information, call intake at 832-393-4301 or the Harris County Area Agency of Aging general number at 800-213-8471. — Cindy George
UPDATE | August 12, 2020, 3:45 p.m.: Harris County Judge Lina Hidalgo provided new guidance for school reopenings on Wednesday, standing by her position to offer virtual-only instruction in lieu of in-person instruction while the community spread of COVID-19 is still uncontrolled.
“The countdown to the first day of school in-person is like a ticking time bomb unless we do this right,” Hidalgo said during a news conference Wednesday afternoon. “We made clear that it’s currently not safe and it won’t be safe any time in the near future to open schools for in-person instruction, but it’s important for not just our school leaders, but our entire community to know when it will be safe and what reopening will look like when that time comes.”
Harris County Judge Lina Hidalgo unveils her “Roadmap to Reopen Schools” during a news conference on Aug. 12, 2020.
The two-pronged approach consists of providing school districts with data from the Harris County threat level system to guide decision making and involving Harris County public health officials in reviewing and approving school districts’ plans. In addition, the guidance also outlines best practices for disinfecting, cohorting, social distancing and mask wearing.
Under Hidalgo’s guidance, school districts are recommended to close in-person instruction and activities as long as there are more than 400 new COVID-19 cases per day, a positivity rate exceeding 5 percent or more than 15 percent hospital bed capacity for COVID-19 patients.
While Gov. Greg Abbott and Texas Attorney General Ken Paxton mandated that only school district officials—not local officials—have the authority to decide when and how to reopen schools, Hidalgo’s plan serves as a common playbook for school districts to use “to put Harris County schools back on track for a realistic, responsible, safe and sustainable reopening,” she explained.
Currently, the threat level remains at red—its highest—with more than 87,000 cases and more than 900 deaths throughout Harris County inclusive of Houston. The threat level system is defined by four sets of indicators: new COVID-19 cases per day in Harris County, positivity rate of tests, percentage of ICU and general beds for COVID-19 and widely available medical countermeasures, such as treatments or vaccine. In order for the threat level to change, all four indicators must be met.
“We can’t grasp at straws looking for a data point or something that will justify an irresponsible reopening of schools right now,” she stressed. “That’s not the point of this or the threat level system. What we can do is present clear research, best practices and informed advice on—when that day comes—how we should reopen.”
Once those metrics are met and the threat level improves, Hidalgo advised reopening using a phased approach at certain capacity levels. For orange, yellow and green, schools should reopen at 25 percent capacity (or 500 people), 50 percent (or 1,000 people) and 100 percent, respectively, as long as cohorting and social distancing can be implemented.
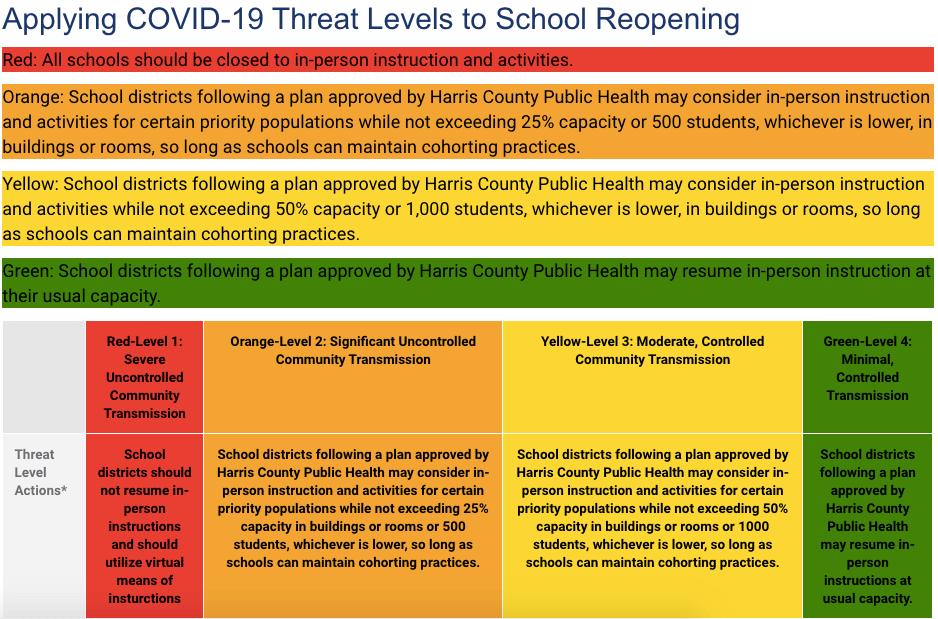
Source: Ready Harris “Roadmap to Reopen Schools”
“I know that in-person learning is vital for the educational development, for the social well-being of children and young adults. I know it’s a crucial lifeline for millions of working parents who are already struggling to get by and can’t work from home,” Hidalgo said. “We will be back in school one day, but we’ll be safe when we do it. What we can’t do is bury our head in the sand. We can’t ignore this. We can’t tap our heels together and wish the current numbers away.”
The Houston Health Department reported today 431 new cases and 12 new deaths, bringing the total to 55,940 cases and 585 deaths. — Shanley Pierce
UPDATE | August 11, 2020, 3:30 p.m.: The Houston Health Department reported 311 new cases of COVID-19 and eight additional deaths today, bringing the city’s totals to 55,509 cases and 573 deaths.
The Texas Medical Center has released a new set of daily metrics and goals to improve COVID-19 tracking efforts in Houston. The new data set includes the effective reproduction rate, daily new cases and test positivity rates across TMC hospital systems.
The effective reproduction rate, denoted as R(t), measures how successfully collective behaviors are slowing the spread of the SARS-CoV-2 virus. If R(t) is above 1.0, the virus spread is increasing; if R(t) is below 1.0, the spread is slowing. The goal for R(t) is to remain below 1.0 for 14 days.
The daily new cases metric shows how many additional positive tests are reported in a day. When the number of new daily cases surpasses 200, contact tracing becomes difficult as does controlling the spread of the virus. The TMC’s goal is for new cases to remain below 200 for 14 days, which would suggest community control of the virus.
The test positivity rate measures the percentage of positive COVID-19 tests out of the total number of COVID-19 tests performed in hospitals in the TMC system. A lowering positivity rate indicates a decline in the spread of the virus; health officials have stated that their goal is to see the positivity rate drop to under 5 percent. The current 7-day average positivity rate for TMC hospital systems is 10.5 percent. Notably, the City of Houston reported yesterday its lowest positivity rate since June 1 with 14.6 percent. Houston health officials calculate the city’s positivity rate based on a rolling 14-day period.
A recent report released by the American Academy of Pediatrics states that between July 9 and August 6, there were 179,990 new cases of U.S. children testing positive for COVID-19—a 90 percent increase over four weeks. As of August 6, more than 380,000 have tested positive for COVID-19 since the onset of the pandemic. “At this time, it appears that severe illness due to COVID-19 is rare among children,” the academy reiterated, but added that states should continue to release detailed information about COVID-19 cases, testing, hospitalizations and mortality by age.
Kaiser Health News is reporting today that the United States has lost more than 900 health workers to COVID-19. The news outlet has partnered with The Guardian to create an interactive database to document and memorialize the deaths of health care workers during the pandemic. Their data shows that, thus far, 62 percent of those who died on the front lines were identified as people of color, and at least 31 percent were reported to have had inadequate personal protective equipment (PPE). The authors added that many of the health care workers who died were immigrants, and at least 35 individuals passed away after federal officials received safety complaints about their workplaces. Notably, the database is a work in progress and new cases are being added weekly.
Finally, President Vladimir Putin announced today that Russia has granted regulatory approval for a COVID-19 vaccine. Reportedly named “Sputnik V,” the vaccine has undergone less than two months of human testing and has not yet completed its final trials. Still, Putin insisted the vaccine is safe and noted that one of his daughters has already received it. The vaccine consists of two serotypes of a human adenovirus, each of which carry an S-antigen of the SARS-CoV-2 virus, which should produce an immune response once injected into the body. It will be administered in two doses. — Alexandra Becker
UPDATE | August 10, 2020, 3:15 p.m.: The United States surpassed 5 million confirmed cases of COVID-19 on Sunday. With 5,063,770 U.S. cases and 19,936,547 global cases, the U.S. now makes up one quarter of the total cases worldwide.
New research projects 300,000 deaths by December
Researchers at the University of Washington’s Institute for Health Metrics and Evaluation (IHME), which has been leading COVID-19 projections and modeling, estimated that—at this rate—the death toll in the U.S. due to the coronavirus could reach close to 300,000 by Dec. 1.
Released Thursday by the institute, the projection would make the coronavirus the nation’s third leading cause of death behind heart disease and cancer.
However, if 95 percent of Americans consistently wear masks in public, that could save more than 66,000 lives, bringing the total number of deaths to 228,271 instead, according to the IHME.
“It appears that people are wearing masks and socially distancing more frequently as infections increase, then after a while as infections drop, people let their guard down and stop taking these measures to protect themselves and others—which, of course, leads to more infections,” IHME director Christopher Murray, M.D., said in a press release. “And the potentially deadly cycle starts over again.”
The IHME model suggests that Texas will need to reimpose mandates, including business closures and stay-at-home orders, in September.
State disaster declaration extended
Gov. Greg Abbott extended Saturday the Disaster Declaration for all counties in the state.
“Renewing this Disaster Declaration will provide communities with the resources they need to respond to COVID-19,” Abbott said in a statement. “I urge Texans to remain vigilant in our fight against this virus. Everyone must do their part to slow the spread of COVID-19 by wearing a mask, practicing social distancing, and washing your hands frequently and thoroughly.”
Abbott initially issued his declaration on March 13. The extension will allow the state to continue providing counties affected by the pandemic with available resources. The governor did not specify an expiration date for the order.
As of Aug. 9, there have been 486,362 cases and 8,459 deaths in the state. Texas also reached its highest seven-day positivity rate at 20.1 percent, according to the Johns Hopkins University COVID tracker.
19 residents die at a Missouri City nursing home as Texas reopens nursing homes to public visitation
A nursing home in Missouri City reported that 19 residents died due to COVID-19. City officials were notified on Aug. 5 of 38 cases, 19 deaths and 24 infected employees at the Paradigm at First Colony.
The outbreak occurred a day before the Texas Health and Human Services issued a new policy allowing limited visitation at nursing homes and assisted-living centers. Given that older adults are at higher risk for severe illness and death from COVID-19, visitors were originally banned from these facilities when the pandemic hit in mid-March in order to protect residents from being infected by the coronavirus.
Under the new policy, public visitation to nursing homes is limited to outdoor areas only and no physical contact between residents and visitors will be allowed. Visitors will be allowed to visit inside long-term care facilities through plexiglass barriers.
Both nursing homes and long-term care facilities will be required to make sure that no staff member has been confirmed positive with COVID-19 in the last 14 days and there are no active cases among residents. Nursing home staff will be tested weekly for COVID-19. — Shanley Pierce
UPDATE | August 7, 2020, 12:30 p.m.: This week, TMC began offering its Coronavirus (COVID-19) Updates in Spanish. More than 20 data slides, refreshed every day, aim to keep citizens informed and prepared with resources, guidelines and ways to be vigilant when it comes to personal health. The “Key Takeaways” slide that sits up front offers a quick view for English and Spanish readers, while other slides offer information on new COVID-19 hospitalizations, TMC bed status, TMC testing capacity and much, much more.
U.S. Rep. Sheila Jackson Lee of Houston
• Congresswoman Sheila Jackson Lee, a Democrat representing Texas’ 18th Congressional District, spoke Friday at a press conference about ongoing negotiations in Washington, D.C., related to the HEROES Act, a bill with a stimulus package that responds to the COVID-19 outbreak and its impact on the economy, public health, state and local governments, individuals and businesses. Lee called for speedy passage of the act.
The first round of $1,200 stimulus checks were sent to eligible Americans starting in March under the CARES Act.
The Health and Economic Recovery Omnibus Emergency Solutions (HEROES) Act, a proposal made by Democratic leadership in the U.S. House of Representatives, asks for a second stimulus package for Americans in need, including municipal workers, postal workers, physicians, nurses, emergency medical technicians and others who provide services in counties affected by COVID-19.
Democrats first asked for $1 trillion to fund the HEROES Act, Lee explained, but have winnowed that request to $925 billion.
“But what is being offered by the Republican Senate is $150 billion,” Lee said. “We can’t do anything with $150 billion. … They need to come back with a message of getting it done.”
Democrats are hopeful that the cash disbursements will include $1,200 for each qualifying adult and child, she added.
• Mayor Sylvester Turner at the same press conference updated Houston’s COVID-19 numbers. The city saw 652 new cases today, for a total of 53,304 cases. Seventeen new deaths were reported in Houston, as well—13 of the individuals were Hispanic, three were Black and one was Asian. Total death count for the city is now 543.
• A new study published in JAMA Internal Medicine found that individuals who tested positive for COVID-19 but were asymptomatic were just as able to spread the virus as individuals who tested positive and were displaying symptoms. The study, which included 303 patients with SARS-CoV-2 infection isolated in a community treatment center in the Republic of Korea, found that the levels of virus in the lungs, noses and throats of asymptomatic patients was basically the same as the levels found in symptomatic patients, though from diagnosis to discharge those levels tended to decrease more slowly in asymptomatic patients. Researchers concluded that “because transmission by asymptomatic patients with SARS-CoV-2 may be a key factor in community spread, population-based surveillance and isolation of asymptomatic patients may be required.”
• The Centers for Disease Control and Prevention offers COVID-19 Travel Recommendations by Country. While the COVID-19 risk is high across most of the globe, the risk is rated “very low” in the following countries: British Virgin Islands, Brunei, Cayman Islands, Dominica, Falkland Islands, French Polynesia, Greenland, Laos, Macau, Mauritius, New Caledonia, Taiwan and Timor-Leste. — Maggie Galehouse
UPDATE | August 6, 2020, 8 p.m.: Al fresco parking lot dining is a new option in Houston to provide relief to restaurants under COVID-19 indoor restrictions and allow more people to patronize these businesses outdoors while physically distancing.
The new “More Space” program, a voluntary effort effective Wednesday, allows each restaurant to convert up to 50 percent of off-street parking spaces into an area to serve food. Social distancing at six feet as well as driveway, pedestrian and ADA (Americans with Disabilities Act) access will remain. Businesses must register for the program, which will last the duration of the COVID-19 space restrictions.
This new idea comes one day before the city reached the morbid milestone of more than 20 reported deaths in one day; 23 to be exact.
https://www.facebook.com/theismailiusa/videos/997183874051490/
The Ismaili Jamatkhana and Center, which has a location in Sugar Land, hosted a live webcast Thursday evening entitled “COVID-19 Pandemic: What we Know and What is Next,” featuring the three physicians who are health authorities in Houston, Harris County and Fort Bend County.
The discussion was moderated by Salim S. Virani, M.D., Ph.D., professor of medicine-cardiology at Baylor College of Medicine, staff cardiologist at the Michael E. DeBakey Veterans Affairs Medical Center and chairman of the Aga Khan Health Board for the United States.
Umair Shah, M.D., MPH, executive director of Harris County Public Health, said we’re at this critical moment in Houston post-shutdown because of the “layering effect” of reopening amid milestones, such as graduations and holidays.
“Then people, frankly, being tired of face coverings and tired of really being at home,” Shah said. Abandoning those preventive measures left us with a higher number of cases, higher positivity rates and an increase in hospitalizations, he added.
Jacquelyn Minter, M.D., MBA, MPH, director of Fort Bend County Health and Human Services, urged people not to get weary.
“Yes, people are tired, but the health care system is tired, as well. The fight has been long and the longer we have to fight, the longer we’re fatigued, as well. The frontline workers—they’re only going to last so long—and I think I see that across the region,” she said. “It’s almost as if now, the energy to keep up the fight—when it’s more important—I just feel that kind of lagging.”
David Persse, M.D., Houston’s health authority, reminded people that the city reported more than 20 additional COVID-19 deaths today.
“This is very serious and we need to focus—and I believe that people will,” he said.
The panelists also discussed the eagerly awaited COVID-19 vaccine and the upcoming flu season. Persse predicted a higher demand for the flu vaccine.
“It’s the development piece that’s absolutely critical, not just for flu vaccine, but COVID-19,” Shah said. “We are hearing from our federal partners, obviously, that there is supposed to be COVID-19 vaccine. … Is it going to be by the end of this calendar year or is it going to be in 2021? The answer is that we just don’t know.”
Minter talked about continuing to be diligent about wearing masks, washing hands and social distancing amid the reality of asymptomatic spread.
“The messaging is about not only yourself, but your friends, your families, your neighbors. All these numbers that we talk about— … each number represents a person. When you’re careless with your behavior, there is a person that’s going to be affected whether you ever feel it or not,” she said. “There are some that are depending on you to have these actions for their lives.”
The discussion also addressed parents who are grappling with K-12 back-to-school, whether in person or virtually.
Persse said it’s true that minors don’t tend to get as sick with the virus, but that’s not the end of the story.
“There are some kids who are going to get sick and, of course, those kids with chronic health issues are at an even greater risk. But, even otherwise healthy kids are still at risk for developing complications—serious complications. The risk is small, but it is absolutely not zero,” he said.
Persse and Shah estimate that there are about 911,000 K-12 students in school districts in Harris County. The city health authority used this metric to illustrate how a small percentage of a really big number is significant when considering that there are about 700 licensed pediatric hospital beds in Harris County, according to the Texas Department of State Health Services.
“So, 700 into 911,000 is .06 percent. You only need that small percentage of the entire student body to get sick enough to need a hospital bed to occupy every single pediatric hospital bed in Harris County,” Persse said. “If we have things go badly with the schools … 100 kids to become critically ill is a tragedy.”
What about a second wave of COVID-19, the financial damage of economic upheaval, the consequences of deferred care or the strain on mental health?
“Don’t lose hope. Feel empowered,” Persse said, emphasizing the “mantra of the mask” and physical distancing. — Cindy George
UPDATE | August 5, 2020, 3:45 p.m.: The Houston Health Department reported 709 new cases of COVID-19 and 14 deaths, bringing the city’s total to 52,320 cases and 503 deaths. The positivity rate is currently at 17 percent; however, the goal is to bring that rate down to 5 percent or below by the end of the month.
Turner announces $20 million for Houston Rental Relief Package
Houston City Council unanimously passed a $20 million rental relief package Wednesday to help residents, especially those from lower income households, who are facing financial hardship due to the coronavirus pandemic.
While the first rental relief package was administered on a first-come, first-served basis, “things are different this time around,” Turner said. Funds will be committed based on a vulnerability prioritization to allow the most needy to move to the front of the line to receive aid.
“We’re taking a look at who’s paying the lowest amount of rent and working up,” Turner said during a news briefing this afternoon. “We want to make sure that people don’t find themselves on the streets.”
Landlords who participate in the program must agree to waive all late fees and interest for the month and allow for interest-free and penalty-free payment plans for any rent due. Landlords also must agree to refrain from evicting tenants through September 2020.
The program will provide a maximum assistance of $2,112 per household. In order to qualify for the rental relief package, tenants must live in the city of Houston and be behind on rent payments for August or previous months due to the economic impact of COVID-19.
The federal CARES Act provided $15 million of the rental relief package and the remaining $5 million came from donors, including the Houston Endowment, the Greater Houston COVID-19 Recovery Fund, the Kinder Foundation and Janice McNair.
Abbott says local school officials, not local health officials, decide when schools can reopen
During a press conference Tuesday, Gov. Greg Abbott stated that local governments do not have the authority to decide how to proceed with school reopenings. Instead, Abbott is leaving those decisions in the hands of local school districts.
“The bottom line is the people who know best … about that are the local school officials,” he said, adding that the state has provided schools with resources and supplies, including more than 59 million masks, 24,000 thermometers, 565,000 gallons of hand sanitizer and 500,000 face shields.
Abbott and other state leaders recently supported a legal opinion by Texas Attorney General Ken Paxton that stated that local health authorities cannot issue sweeping orders for school closures. The opinion limited by statute the role of local health authorities to address specific outbreaks of the disease.
“Education of our children is an essential Texas value and there is no current statewide order prohibiting any school from opening,” Paxton said. “While local health authorities may possess some authority to close schools in limited circumstances, they may not issue blanket orders closing all schools on a purely preventative basis. That decision rightfully remains with school system leaders.”
Paxton’s legal opinion prompted the Texas Education Agency to withdraw its previous policy of funding schools under a local health mandate. Now, if school districts choose to remain closed and opt for remote learning, they can only receive state funding for up to eight weeks. Schools can apply for waivers if they request more time. — Shanley Pierce
UPDATE | August 4, 2020, 3:45 p.m.: The Houston Health Department is reporting 715 new cases of COVID-19 today, bringing the city’s total to 51,611. The City of Houston’s death toll has also increased by 11, bringing that total to 489.
During an afternoon press briefing, Harris County Judge Lina Hidalgo said the county is reporting the highest case count today since the beginning of the pandemic, with 723 new cases outside the City of Houston. The county is also reporting 11 new deaths.
Hidalgo said that the county received 30,000 expedited tests from the federal government and would be transitioning Harris County Public Health’s testing locations at Ken Pridgeon Stadium and the San Jacinto College Central Campus to surge testing sites beginning Thursday.
Texas Gov. Greg Abbott also announced today that the McAllen Convention Center would be converted into a health care facility to help meet the region’s needs as Rio Grande Valley-area hospitals are at or over capacity due to an influx of COVID-19 patients.
The City of Houston’s Department of Neighborhoods has announced a new way for Houstonians to stay informed about COVID-19 recovery resources, essential city services and seasonal advisories. The program, called Neighborhood Updates, will send information to the public via voice and text messages in both English and Spanish. Citizens—especially seniors, persons with disabilities who require voice or text communications, and individuals who prefer information in Spanish—are encouraged to subscribe to Neighborhood Updates by calling 311.
Yesterday, Reuters reported on the promise of manufactured antibodies in the fight against COVID-19. Manufactured antibodies, also known as monoclonal antibodies, are created in labs to mimic naturally-occurring antibodies, which are developed as part of a body’s immune response against a virus. Antibodies recognize viruses and latch onto them to prevent replication and spreading throughout a person’s body. The therapy has been used successfully against cancer and other diseases.
Researchers at Baylor College of Medicine’s Human Genome Sequencing Center and the Alkek Center for Metagenomics and Microbiome Research are now partnering with local public health departments to provide polymerase chain reaction (PCR) testing for tens of thousands of COVID-19 samples. Baylor has been one of the testing providers for Harris County Public Health since May and has already helped process more than 30,000 samples.
The New York Times published a story yesterday stating that infectious diseases such as tuberculosis, HIV and malaria are “making a comeback” as a result of the COVID-19 pandemic’s impact on global resources. The article quotes Pedro L. Alonso, M.D., Ph.D., director of the World Health Organization’s global malaria program, as saying that the pandemic risks “derailing all our efforts and taking us back to where we were 20 years ago.” The authors of the article noted that part of the issue is that lockdowns, including those in parts of Africa, Asia and Latin America, “have raised insurmountable barriers to patients who must travel to obtain diagnoses or drugs,” and that many people who can access clinics have avoided them for fear of contracting COVID-19.
In other news, the obituary of a man from Jefferson, Texas—who died after contracting COVID-19—made headlines for its no-holds-barred sentiments about individuals who refuse to wear masks.
“Dave did everything he was supposed to do, but you did not,” his wife Stacey Nagy, wrote in the obituary. “Shame on all of you, and may Karma find you all!”
David W. Nagy, 79, died on July 22. — Alexandra Becker
UPDATE | August 3, 2020, 6:15 p.m.: Mask up or pay up in Houston.
Mayor Sylvester Turner has directed police to issue citations carrying $250 fines for anyone not wearing a face mask or facial covering as required by the state’s mandatory mask order. Officers also may issue warnings and won’t ticket those who are not wearing a mask but meet exemption criteria.
“July was a tough month for us,” the mayor said. “Our positive cases and the number of deaths doubled compared to the four previous months, March through June. … It is imperative that we bring the number of people who are testing positive and dying down as much as possible in the month of August.”
Today, the Houston Health Department reported another 1,104 new cases and six new deaths, all Hispanic individuals. The mayor noted the heavy impact the virus has had on the Latinx community.
Data improving: Hospitalizations in Houston have dropped and the positivity rate of COVID-19 tests also have improved from 25.9 percent in late June and early July to 17.6 percent today. The goal is 5 percent or below.
Firefighter dies: COVID-19 has claimed the life of a second Houston firefighter.
Gerado “Jerry” Pacheco, a 17-year veteran of the Houston Fire Department, died from complications of coronavirus on Monday morning, Houston Fire Chief Samuel Peña announced. The 50-year-old firefighter paramedic was assigned to HFD Station 101 in Kingwood and has a son, Justin Pacheco, who is also a Houston firefighter.
HFD Captain Leroy Lucio died on July 20 after a monthlong battle with COVID-19.
More Mask Up: The nation’s physicians, nurses and hospitals have united for their own #MaskUp campaign urging Americans to follow the science and the advice of medical professionals to stop the spread of COVID-19. The American Hospital Association, the American Medical Association and the American Nurses Association are providing images and messages for all to share on social media.
Food relief: Families who lost access to free or reduced-price school meals amid campus closures during the 2019-2020 academic year are eligible to receive a one-time benefit of up to $285 for each child. The extended deadline to apply is August 21.
Visit yourtexasbenefits.com/Learn/PEBT for an online application for the Pandemic Electronic Benefit Transfer (P-EBT). The $1 billion benefit program was approved by the U.S. Department of Agriculture to help eligible families buy food during the COVID-19 pandemic. The benefit will be issued on an EBT card, which can be used as a debit card to assist families in buying food from any retailer that accepts the Texas Lone Star Card. — Cindy George
UPDATE | July 31, 2020, 4 p.m.: On this final day of July, the City of Houston reported 18 deaths due to COVID-19—the highest daily death total since the pandemic arrived. That brings the total number of deaths from COVID-19 to 450. In addition, the city reported 1,554 news cases today, bringing the total number of cases in Houston to 46,969.
“With all due respect to the state attorney general, there is no way under the sun that I would allow my child to go to school if these numbers are the same or greater by the end of August,” Mayor Sylvester Turner said in an afternoon press conference. “These numbers must come down.”
Turner announced a second rental assistance program for Houstonians struggling as a result of financial hardships caused by COVID-19. The $19 million rent relief package will go to the most vulnerable people; it will be “a lifeline to those facing immediate eviction,” Turner said.
Of that $19 million total, $15 million comes from CARES Act funding, $2 million from the Houston Endowment, $1 million from the Greater Houston COVID-19 Recovery Fund and $1 million from the Kinder Foundation.
This is the second rental assistance package from the city; Houston offered $15 million in CARES Act money in May.
“We realize without significant rental assistance funding from Congress, our efforts will not be nearly enough,” Turner said. I am calling on the state of Texas and the federal government to help. Cities cannot do this alone.”
At the same press conference, Houston health authority David Persse, M.D., said that the number of individuals being tested for COVID-19 in the Houston area is declining. He and the mayor encouraged citizens to continue to get tested at locations throughout Harris County.
• Rice University students have started to return to campus for a fall semester that will prioritize the health and safety of everyone in the academic community. Students generally have the option of attending classes either in person or online; about 20% of undergraduate students plan to attend their classes remotely. Overall, the university expects about 40% of its undergraduate students to live on campus.
• A new study published in JAMA Pediatrics found that children under age 5 have high amounts of SARS-CoV-2 viral RNA in their noses and throats, as compared to older children and adults.
“Young children can potentially be important drivers of SARS-CoV-2 spread in the general population,” authors of the study concluded. “Behavioral habits of young children and close quarters in school and day care settings raise concern for SARS-CoV-2 amplification in this population as public health restrictions are eased. In addition to public health implications, this population will be important for targeting immunization efforts as SARS-CoV-2 vaccines become available.” — Maggie Galehouse
UPDATE | July 30, 2020, 7:15 p.m.: As Houston continues to endure rising COVID-19 cases, exceeding 1,000 daily, and a day of double-digit deaths, there’s a new strategy to stem the tide in August called “Better. Together.”
The multilingual and data-driven public health education campaign, with door-to-door neighborhood canvassing led by the Houston Health Department (HHD), aims to empower Houstonians with COVID-19 prevention information to reduce the city’s testing positivity rate from its current 23 percent to 5 percent. The effort was officially presented to the public on Thursday by Mayor Sylvester Turner and will target high-positivity areas and populations.
“One of the biggest hurdles we face is getting factual, potentially lifesaving information into the hands of the people who need that information the most,” Turner said at his Thursday news conference. “The campaign includes broad city-wide messaging across TV, radio, print, digital, outdoor and more. In fact, tomorrow, the Houston Health Department will have teams of workers spreading out across neighborhoods to place door hangers and talk to people. … The public health crisis needs more direct communication with the public, especially in neighborhoods that have been hit hardest by COVID-19.”
On Thursday, the city reported 1,304 new cases and 15 deaths (nine were Hispanic individuals), bringing Houston’s total to 45,415 cases and 432 deaths. On Wednesday, there were 1,045 new cases. In July alone, 200 people have died in Houston from COVID-19.
Earlier this month, HHD launched “Todos juntos. Mejor.” (All together. Better.)—an emergency Hispanic outreach campaign in Spanish, mainly on social media.
“Our goal in August is to make progress in the fight against COVID-19,” Turner said. “This is the month that we turn this around—not just in our hospitals—but we turn this virus around in our community.”
Though hospitalizations have “plateaued,” the mayor said, “community spread” continues to increase. He reiterated the COVID-19 precautions to mask up and engage in social distancing with proper hygiene.
“The goal of Better Together is to empower Houstonians with the knowledge and skills to protect their families and community from COVID-19. In order to bring our positivity rate down, we must continue to go directly into communities,” said Faith Foreman-Hays, DrPH, MPH, chief of HHD’s Office of Chronic Disease, Health Education and Wellness. “This means educating people in their homes, apartments, schools, parks, businesses, houses of worship, restaurants and other places … with special focus in high-positivity communities and populations.”
Testing has dipped at the city’s free sites, so residents are encouraged to max out those opportunities. Visit houstonemergency.org/covid-19-testing for information about the city’s free testing sites and partner testing locations as well as houstoncovid19recovery.org for comprehensive COVID-19 information. — Cindy George
UPDATE | July 29, 2020, 4:35 p.m.: As of today, at least 150,000 people in the U.S have died from COVID-19, with at least 1,000 deaths every day this week, according to The New York Times. The Houston Health Department is reporting 1,045 new cases and nine additional deaths today, bringing the city’s total to 44,111 total confirmed cases and 417 deaths.
The New York Times also reported yesterday that at least 21 states could be classified as “red zones” for rising COVID-19 outbreaks. According to an article published today in The Guardian, the United States experienced the “deadliest day of the summer in the last 24 hours.” A tally by Reuters showed more than 1,200 deaths from COVID-19, which is the highest daily count in the country since the month of May.
The rising numbers support messaging from the World Health Organization, which yesterday described the pandemic as “one big wave,” and reiterated the general consensus that the SARS-CoV-2 virus does not seem to be seasonal like, say, influenza. Experts warned the public not to become complacent during the summer months, saying simply: “This virus likes all weather.”
Amid daily debates about reopening schools, STAT news reported on a study published today in the Journal of the American Medical Association (JAMA) which provided evidence that closing schools earlier this year led to a drastic decrease in COVID-19 infections and fatalities. The author of the STAT news story, Eric Boodman, wrote that “the point at which officials made that call mattered: Those states that adopted the policy while few people were testing positive saw a correlated flatter curve of cases.”
Adding fuel to the school reopening fire: A study out today ranks The University of Texas at Austin as having the most cases of COVID-19 outbreaks among all U.S. colleges.
It is also reported that Texas Rep. Louie Gohmert, who has been outspoken about his refusal to wear a mask, has tested positive for COVID-19.
In other news, The Menninger Clinic recently launched a maternal mental wellness program for mothers struggling with mental health issues during the pandemic, a first of its kind in Texas. The Menninger Moms Program is a virtual program designed by moms, for moms, which offers a customized care package, a la carte services and an eight-week “Connecting During a Crisis” therapy group, which is led by a psychologist and tackles topics like managing guilt and crisis survival. The program also offers a free virtual support group open to all moms in Texas, which focuses on building community and helping mothers feel supported.
Finally, a study published yesterday in the New England Journal of Medicine described promising results of an mRNA vaccine against the SARS-CoV-2 virus in non-human primates. The researchers, who tested mRNA-1273, a vaccine encoding the prefusion-stabilized spike protein of SARS-CoV-2, found that it “induced robust SARS-CoV-2 neutralizing activity, rapid protection in the upper and lower airways, and no pathologic changes in the lung.” — Alexandra Becker
UPDATE | July 28, 2020, 4:46 p.m.: The Houston Health Department reported 864 new cases of COVID-19 and eight new deaths today, bringing the city’s total to 43,066 cases and 408 deaths.
Texas’ tally of COVID-19 deaths increases 12 percent after state officials look at death certificate data
As a result of Texas health officials changing their reporting method, the revised number of COVID-19 deaths in the state increased by more than 600, showing that more than 12 percent of the total number of deaths had previously gone unreported.
Public health experts raised concerns that many deaths were not being reflected in the state’s official death toll, prompting the Texas Department of State Health Services (DSHS) to revise its approach. DSHS is now using death certificates that indicate COVID-19 as the cause of death to calculate the total fatalities in the state instead of relying on local and regional public health departments to report deaths. Identifying COVID-19 deaths through death certificates will ensure faster and more consistent reporting, the department said.
Compared to the 5,038 deaths the state originally reported on Sunday, the department announced that there are now 5,713 deaths in Texas, including 44 newly reported fatalities, according to death certificate data.
Two coronavirus vaccines enter final phase of testing
Biotechnology company Moderna Therapeutics and pharmaceutical powerhouse Pfizer announced Monday that they started the final phase of testing for the first U.S. coronavirus vaccines.
At 6:45 a.m. Monday, a volunteer in Savannah, Georgia, was injected with the coronavirus vaccine developed by Moderna as part of a highly anticipated phase 3 clinical trial to test the safety and efficacy of an experimental coronavirus vaccine.
In collaboration with the National Institutes of Health, the double-blind study will enroll 30,000 healthy volunteers from 89 sites across the country, with half of the participants receiving the vaccine candidate and the other half receiving a placebo. Each group will be injected twice, each shot administered 28 days apart.
During a news briefing, Anthony Fauci, M.D., the director of the National Institute of Allergy and Infectious Diseases, said he expects full enrollment will be completed by the end of summer, with early results of the study in November.
Pfizer also announced Monday that it has launched its phase 3 for a coronavirus vaccine candidate, with the first volunteer receiving the injection at the University of Rochester. In partnership with German biotechnology company BioNTech, the study will include 30,000 participants the United States, Brazil, Argentina and Germany.
Three other companies—Novavax, Johnson & Johnson and AstraZeneca, in partnership with the University of Oxford—will begin their respective phase 3 trials soon.
Two German studies show long-term heart damage after COVID-19
Two recent studies from Germany, published Monday in JAMA Cardiology, show that COVID-19 can leave long-term damage on the heart on recovered patients.
One study looked at the magnetic resonance imaging (MRI) tests of 100 patients who had recently recovered from COVID-19 and found that 78 of them had ongoing cardiac complications and 60 had ongoing myocardial inflammation, independent of preexisting conditions and severity of the illness.
The other study analyzed the autopsy results of 39 people and revealed high viral loads of SARS-CoV-2 in the hearts of 24 patients.
While further studies need to be done to better understand the long-term effects of COVID-19, the results of the two studies suggest that the virus could have a larger impact on the heart that initially believed and could lead to cardiac damage and heart failure. — Shanley Pierce
UPDATE | July 27, 2020, 4:15 p.m.: Over the weekend, Texas surpassed 5,000 deaths from COVID-19, with 1,000 of those deaths reported in just six days. As of today, the City of Houston has reached the grim milestone of 400 total deaths after reporting nine additional fatalities. The Houston Health Department is also reporting 325 new cases of COVID-19 today, bringing the city’s total to 42,202.
On Saturday, Harris County Precinct 5 deputy constable Mark Brown died after a two-month battle with COVID-19. The 53-year-old had served in law enforcement for 23 years.
During an afternoon press conference, Mayor Sylvester Turner noted that in the month of July alone, approximately 22,000 people have tested positive for COVID-19 in Houston. He also displayed a chart illustrating the progression of COVID-19 deaths, by month of announcement, in the city (see below). In March, four people were known to have died from COVID-19; in April, 52 deaths were reported; in May that number rose to 73; in June, there were 95 deaths; and in July there have been a total of 176 as of July 27.
“It reflects that there is significant community spread and it reflects the fact that more people are continuing to die as we proceed,” Turner said. “What will be needed in order to slow that progression, to stop the number of people who are dying, is that we must—we must—collectively, not individually, put on our masks, social distance, practice proper hygiene and take this virus very seriously.”
Houston’s health authority, David Persse, M.D., also reported on the city’s positivity rate, which is currently 23.3 percent. Persse said this is still considered to be “extremely high.”
Turner also announced that the 10th annual Back to School Fest presented by Shell will follow a drive-thru format this year at NRG Stadium.
“Just like the start of the school year, this year’s Back to School Fest will be different than in previous years, but no less important,” Turner said.
The event will take place in the yellow lot at NRG Stadium over two days: Friday, August 7, and Saturday, August 8. Backpacks stuffed with school supplies will be available for 25,000 elementary school-aged children, as will food for their families provided by the Houston Food Bank. The Mayor’s Health Equity Response (H.E.R.) Task Force will also be distributing masks during the event. Families can register their children in grades K-5 at houstontx.gov/btsf.
Houston-based company and TMCx alumni Vitls recently won a $50,000 grant from the National Capital Consortium for Pediatric Device Innovation during a “Make Your Medical Device Pitch for Kids!” competition focused on COVID-19-related devices. Vitls provides continuous monitoring technology paired with cloud-based data analysis to enable quick and precise decision-making if a patient’s vitals begin to deteriorate.
Finally, as the development of a COVID-19 vaccine remains a top priority worldwide, a new study shows a surprising benefit to the annual flu vaccine. After analyzing more than 300,000 anonymous health records from 600 hospitals, researchers from McGovern Medical School and the UTHealth School of Biomedical Informatics have identified a connection between getting a flu vaccine and a lower risk of developing Alzheimer’s disease. The study, which was presented at the 2020 Alzheimer’s Association International Conference, showed that at least one flu vaccine was associated with a 17 percent reduction in Alzheimer’s incidence, and that more frequent flu vaccination was associated with another 13 percent reduction. – Alexandra Becker
UPDATE | July 24, 2020, 2:30 p.m.: To protect the local community and limit the risk of exposure to COVID-19, public and non-religious private schools in Houston and Harris County must not reopen for on-campus, face-to-face instruction until after Sept. 7, 2020, according to control measures released today by Harris County Health Authority Umair Shah, M.D., MPH, and City of Houston Health Authority David Persse, M.D. Other new measures included in the Joint Control Order:
- virtual instruction will remain consistent with academic plans of individual districts or schools
- school-sponsored activities and events must not take place in person, on or off campus, until school systems resume on-campus instruction
• A new report from the CDC finds that a handful of underlying medical conditions are extremely prevalent among United States COVID-19 patients that require hospitalization and ICU admission. The underlying medical conditions include chronic obstructive pulmonary disease, heart conditions, diabetes mellitus, chronic kidney disease and obesity. The report examined data from 3,142 U.S. counties.
“The median county prevalence of any of five underlying medical conditions that increase the risk for severe COVID-19–associated illness was 47.2%, and prevalences were higher in counties in the southeastern United States and in more rural counties,” the report states. “These county level estimates can be used together with data on hospitalizations, ICU admissions, and ventilator use among COVID-19 patients with underlying conditions when planning for mitigation efforts and additional resource investment, including hospital beds, staffing, ventilators, and other medical supplies that might be needed to treat persons with underlying medical conditions, should they become ill with COVID-19.”
• On Friday morning, Houston Mayor Sylvester Turner visited staff at Fallbrook Church on Walters Rd., one of the two COVID-19 test sites established by New York Governor Andrew Cuomo, to thank workers for their help during the spike in COVID-19 cases in Houston. Operated by New York state health workers and public health experts, the two test sites are part of Cuomo’s effort to give back to those cities that stepped up to provide assistance when New York was a COVID-19 hotspot.
•Launched earlier this week, the COVID-19 Law Lab is an initiative that “gathers and shares legal documents from over 190 countries across the world to help states establish and implement strong legal frameworks to manage the pandemic,” according to a press release from the World Health Organization (WHO). “The goal is to ensure that laws protect the health and wellbeing of individuals and communities and that they adhere to international human rights standards.”
The COVID-19 Law Lab is a joint project of the WHO, the United Nations Development Programme (UNDP), the Joint United Nations Programme on HIV/AIDS and the O’Neill Institute for National and Global Health Law at Georgetown University.
“Laws and policies that are grounded in science, evidence and human rights can enable people to access health services, protect themselves from COVID-19 and live free from stigma, discrimination and violence,” says Achim Steiner, UNDP Administrator, in a statement. “The COVID-19 Law Lab is an important tool for sharing good practices on laws and policies.”
• Curbing wildlife trafficking and the destruction of tropical forests could help prevent future pandemics, says a new paper by a team of scientists including Rice University’s University’s Ted Loch-Temzelides.
“Zoonotic viruses infect people directly most often when they handle live primates, bats, and other wildlife (or their meat) or indirectly from farm animals such as chickens and pigs,” says the paper, published July 23 in Science. “The risks are higher than ever as increasingly intimate associations between humans and wildlife disease reservoirs accelerate the potential for viruses to spread globally.”
The paper goes on to argue that the costs associated with preventing deforestation would be “substantially less” than the costs of dealing with the economic fallout and the loss of so many lives during a full-blown pandemic.
While the cost of COVID-19 could reach $15 trillion worldwide, governments could help prevent this sort of situation from occurring again by investing as little as $22 billion a year in programs to suppress wildlife trafficking and stop the destruction of tropical forests, the paper’s authors argue. — Maggie Galehouse
UPDATE | July 23, 2020, 6:30 p.m.: The Houston region is headed in the wrong direction on COVID-19. The grim news was reiterated on social media Thursday by the area’s top government leaders: Harris County Judge Lina Hidalgo and Houston Mayor Sylvester Turner.
On Wednesday, Harris County reported 671 cases—the largest single-day number since the beginning of the pandemic.
“Yesterday we set a terrible record,” Hidalgo wrote. “If we want to get our lives back on track we need to keep working together to crush the curve.”
On Thursday, Houston reported 919 new cases—triple the daily number, 300, that Turner has said is manageable for adequate contact tracing. The city also added 11 deaths today, bringing the total to 357. There’s more information available on the Harris County/Houston COVID-19 Dashboard.
Both Hidalgo and Turner have asked Gov. Greg Abbott for a two-week shutdown to “reset” the area. The mayor is also asking for some backup, specifically for “the medical community to be more vocal on whether additional measures are needed to reverse course.”
Gulf Coast Regional Blood Center has been overwhelmed by donors who may have antibodies for SARS-CoV-2, the virus that causes COVID-19, in their plasma that can help others recover.
“Due to the overwhelming response for antibody testing, results are delayed. We are processing your tests and will post the results to your Digital Donor account as soon as they are complete. The Blood Center will invite donors who test positive for the antibodies to return and give convalescent plasma to help patients recover in local hospitals,” the center’s website said.
To schedule an antibody test or blood donation, visit giveblood.org to find the dates and times of area blood drives or to make an individual appointment at a blood center location.
The National Institutes of Health (NIH) is exploring antibodies and other treatments for COVID-19 as well as more accurate and faster testing.
According to STAT News, new NIH clinical trials are hoped to “expand what for now remains a limited arsenal of therapies to help people with the disease.”
Among the trials are “studies of antiviral monoclonal antibodies to treat COVID-19 in both hospitalized patients and patients who can be treated at home; studies of drugs to quell overreaction of the immune system that the agency has picked from dozens of approved treatments; and studies of blood thinners in very sick COVID-19 patients to prevent problems caused by blood clots. Those treatment studies will be on top of the work that the NIH is also doing on vaccines, including the COVID-19 vaccine being developed by Moderna Therapeutics,” STAT reported.
The Alief area food and mask drive scheduled for July 25 by Turner and the city’s Health Equity Response (H.E.R.) Task Force at Notre Dame Catholic Church has been postponed because of expected rain and flooding Saturday morning from a tropical depression. — Cindy George
UPDATE | July 22, 2020, 3:30 p.m.: The Houston Health Department reported today 773 new cases and eight new deaths, bringing the total to 38,516 cases and 346 deaths.
During a news conference this afternoon, Houston Mayor Sylvester Turner announced that there is a modest drop in the city’s hospitalizations and positivity rate. The positivity rate is currently at 25 percent.
“Although we are seeing some slight improvement in hospitalization admissions and positivity rate, we still have a long way to go,” Turner said.
Turner added that the goal is “not just to flatten the curve or bend the curve, but to drive it all the way down.” In order for the city to manage the virus effectively, the positivity rate must be at 5 percent or less.
Prevalence of COVID-19 ranges from 6 to 24 times higher than official count
The actual number of COVID-19 cases may be significantly greater than we realize. According to a study by the CDC, researchers estimated that there could be six to 24 times more infections than the number of reported cases. In seven of the states in the study, the estimated numbers of infections were 10 times more than what had been confirmed.
Published Tuesday in JAMA Internal Medicine, the study analyzed SARS-CoV-2 antibodies in blood samples from more than 16,000 people of all ages from 10 states, (California, Connecticut, Florida, Louisiana, Minnesota, Missouri, New York, Pennsylvania, Utah and Washington). Because the study uses old data collected between March 23 and May 12, the current numbers would be higher due to the recent surge in new cases.
Remote monitoring supports COVID-19 patients at home
The University of Pennsylvania Health System developed an automated program, called “COVID Watch,” that uses twice-a-day check-ins via text message and telemedicine support to provide confirmed or suspected COVID-19 patients with at-home care.
Of the 3,000 people in the pilot program, 83 percent of them were able to manage their illness using COVID Watch without requiring in-person care.
With the coronavirus pandemic forcing medicine to evolve and adapt to telemedicine approaches, companies are looking at ways to make their platforms work for other conditions in the future.
“While we hope there will be no long-term need for COVID Watch, we believe that its broad uptake and support sets an example for future automated programs that facilitate patient care and communication while increasing efficiency,” the team that developed COVID Watch said.
Houston’s Health Equity Response Task Force distribute COVID-19 food and supplies
On June 25, Turner and the city’s Health Equity Response (HER) Task Force will be joined by physician volunteers and faith leaders to deliver free food, milk, masks and educational pamphlets to families in Alief.
The event will distribute between 1,000 and 2,000 care packages to help alleviate health disparities in the Alief community and will be held at the Notre Dame Catholic Church (7720 Boone Road, Houston, Texas 77072) on Saturday, July 25 from 9 a.m. to 11 a.m. — Shanley Pierce
UPDATE | July 21, 2020, 12:30 p.m.: More than 4,000 Texans have died of COVID-19, according to the Texas Department of State Health Services. Yesterday afternoon, the state reported a total of 4,020 deaths and more than 150,000 estimated active cases.
• Gulf Coast Regional Blood Center needs between 800 and 1,000 daily donations to provide blood and blood products to 170 hospitals and institutions across the region. To that end, The Health Museum, 1515 Hermann Drive, is hosting a community blood drive and providing free antibody testing on Thursday, July 23, and Friday, July 24, from 10 a.m. to 2:30 p.m. Donations are by appointment only. Visit https://www.giveblood.org/the-health-museum/ to make an appointment. Each donor will receive a free beach towel.
• The Lancet medical journal yesterday published results from studies of two different vaccines being considered to quell the spread of COVID-19, one of which showed promising results.
A randomized control trial at five different centers in the United Kingdom showed that vaccine candidate ChAdOx1 nCoV-1, being developed at Oxford University, was safe and tolerated given as a single dose, with adverse effects in the mild to moderate range. A single dose “elicits an increase in spike-specific antibodies by day 28 and neutralising antibody in all participants after a booster dose,” researchers found. “The preliminary results of this first-in-human clinical trial supported clinical development progression into ongoing phase 2 and 3 trials.”
• Houston Mayor Sylvester Turner on Monday offered prayers and condolences to the families of two Houston Public Works employees who died of COVID-19 last week. Natarvia Robertson worked in Customer Account Services and Michael Sanchez worked in Transportation & Drainage Operations.
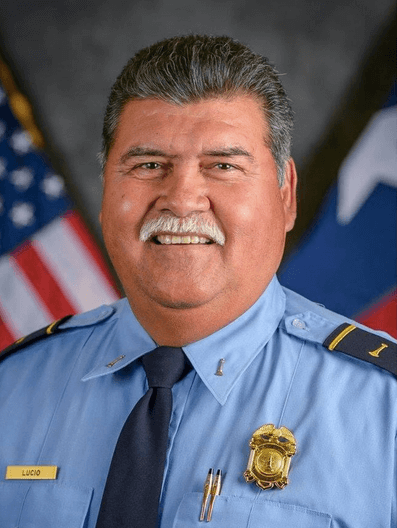
Houston Fire Capt. Leroy Lucio died of COVID-19.
Turner also released a statement on the death of Houston Fire Capt. Leroy Lucio, who perished from COVID-19: “I ask the City of Houston to join me in praying for Capt. Leroy Lucio’s family. His death leaves a void in the department and in the hearts of the men and women that he mentored and supervised during his 30 year career in the Houston Fire Department. We are grateful for his service to the city. May he rest in peace.” — Maggie Galehouse
UPDATE | July 20, 2020, 3:40 p.m.: The Houston Health Department is reporting 884 new cases of COVID-19 today, bringing Houston’s total count to 36,985. The City of Houston is also reporting seven additional deaths, bringing that total to 329. Six of the seven newly reported deaths were Hispanic individuals, including one in his 40s and another in his 50s.
“As a city, we are asking everyone to continue to take this virus very seriously so that we can do everything we can to slow the progression of this virus in the month of July,” said Mayor Sylvester Turner during an afternoon press briefing. “That is our goal—to flatten and to start reducing this curve in the month of July.”
Mayor Sylvester Turner also reported that 224 municipal employees have tested positive for COVID-19 and that as a result, city services may be impacted. Last week, two City of Houston employees died in a 24-hour period from complications related to COVID-19.
Worldwide, there have been more than 14.4 million cases and 600,000 deaths reported, with 140,000 deaths in the U.S. alone.
On Saturday, the FDA issued an emergency use authorization (EUA) for a COVID-19 test that pools samples from a group of up to four individuals to determine the presence of the SARS-CoV-2 virus. According to a statement released by the FDA, sample pooling allows for more testing throughput while using fewer resources:
“The samples collected from these four individuals are then tested in a pool or “batch” using one test, rather than running each individual sample on its own test. If the pool is positive, it means that one or more of the individuals tested in that pool may be infected, so each of the samples in that pool are tested again individually,” the statement read.
Researchers at Baylor College Medicine are currently recruiting health care workers who treat COVID-19 patients in the Houston area for a clinical trial to determine if an existing tuberculosis vaccine may be effective in preventing COVID-19. Participants will be given either the bacille Calmette-Guerin (BCG) vaccine or a placebo, and will be asked to report progress for six months. Health care workers interested in participating should email Andrew DiNardo, M.D., at dinardo@bcm.edu.
The Texas Tribune is reporting that some critically ill COVID-19 patients in Texas are being forced to travel relatively long distances for care due to increased demands on local resources as new regions continue to crop up as COVID-19 clusters. The authors of the story wrote that, “Stretches of South Texas, especially the Rio Grande Valley and the Coastal Bend, have seen coronavirus infections spread so quickly in recent weeks as to push local hospitals to their limit.” The experts interviewed for the story are blaming numerous and widespread smaller gatherings on spreading the disease.
The Houston Health Department and its agency partners have announced the schedule for free COVID-19 testing sites for this week. As a reminder, there is no cost associated with a test at these sites and they do not require proof of residency, citizenship or insurance. Full information about each site, including locations, phone numbers and whether registration is required ahead of time, can be found here.
It was also reported on Saturday that U.S. Representative John Lewis passed away on July 17 at the age of 80 after a months-long battle with pancreatic cancer. The civil rights leader and longtime congressman was born to sharecroppers and was one of the original Freedom Riders. He survived a brutal attack by police officers during the legendary civil rights march in 1965 in Selma, Alabama and is widely considered to be an American hero for his lifetime of work fighting segregation, racism, prejudice and injustice. — Alexandra Becker
UPDATE | July 17, 2020, 4 p.m.: Over the last 24 hours, two municipal employees passed away due to COVID-19, said Houston Mayor Sylvester Turner at an afternoon press conference.
Harris County Public Health reported 986 new cases of COVID-19 in Houston today, bringing the total of active cases to 34,681. Eleven new deaths from COVID-19 were reported in the city today, as well, increasing the total to 315, Turner said. Four of the individuals who died were Asian, three were African American and four were Hispanic.
Yesterday, 154 people in Texas died of COVID-19—a state record, the mayor added.
“The virus in our community is running rampant,” Turner said. “I am asking you to stay home.”
Turner reminded listeners to “mask up” and make sure every mask they wear covers their nose and mouth.
Houston Mayor Sylvester Turner speaks at a press conference on July 17, 2020.
Houston Health Department’s David Persse, M.D., provided additional data on the virus in Houston.
“Seven-hundred people in Harris County are in intensive care units, fighting for their lives,” Persse said. “You may not know anyone who’s sick. You may not know anyone who has died. Yet.”
• In a letter to National Institutes of Health (NIH) president Francis Collins, M.D., dozens of scientists and physicians from the United States and around the world called for COVID-19 challenge trials to help accelerate vaccine development.
Human challenge trials allow volunteers to be infected with COVID-19 in order to speed up vaccine testing. Trial participants should be relatively young and in good health, the letter notes, and should receive the highest quality medical care and frequent monitoring.
“Human challenge trials can provide information much faster than conventional efficacy trials, which take months longer,” the letter states. “In such trials, volunteers still receive the vaccine candidate or a control. Instead of resuming life as usual and waiting to ‘catch a virus,’ volunteers are deliberately exposed to the pathogen under controlled conditions. Beyond being faster than conventional trials, a challenge test is likelier to conclude with interpretable results, e.g. should the presence of virus around the study site begin to fade over time.”
The 125 signatures on the letter include the following Texas-based individuals and organizations: Scott Aaronson, the David J. Bruton Centennial Professor of Computer Science, University of Texas at Austin; David Zuckerman, Professor of Computer Science, University of Texas at Austin; and Ambassador James Glassman, Founding Executive Director at the George W. Bush Institute in Dallas.
• NPR reports that both Target and CVS are requiring customers to wear masks, in an effort to stem the spread of the coronavirus.
“With the recent spike in COVID-19 infections, we’re … requiring all customers to wear face coverings when entering any of our stores throughout the country effective Monday, July 20,” CVS Health Chief Operating Officer Jon Roberts said in a statement released Thursday. “To be clear, we’re not asking our store employees to play the role of enforcer. What we are asking is that customers help protect themselves and those around them by listening to the experts and heeding the call to wear a face covering.” — Maggie Galehouse
UPDATE | July 16, 2020, 5:15 p.m.: Houston health officials reported yesterday 16 new deaths related to COVID-19. This is the largest single-day record to date, bringing the total number of deaths due to the coronavirus to 295 and confirmed cases to 32,693.
“The reason, we believe, that Houston’s death rate is so far behind many other locations is because up until recently, Houstonians did a terrific job of slowing down the virus,” David Persse, M.D., the city’s health authority, said during a press briefing yesterday afternoon. “People are talking about this being a second wave, and I said, ‘This isn’t a second wave.’ What happened back in early March, that was a ripple. What we’re experiencing now is wave. We’ve never had the first wave because Houstonians did such a great job of stopping and slowing down the virus.”
Death rates will continue to rise if people fail to wear face coverings, maintain social distance and wash their hands, Persse added.
New York Gov. Cuomo sends COVID-19 resources to Houston
New York Gov. Andrew R. Cuomo announced today that he is sending resources to Houston to support two new free COVID-19 testing sites in the city.
Cuomo sent 19 clinical staff, five support staff and additional testing supplies for the two testing sites, which will remain open for two weeks.
“When New York went through the unprecedented challenge and unimaginable tragedy of COVID-19’s apex in the state, states throughout the country provided supplies, ventilators and personnel during our time of greatest need,” Cuomo said in a statement. “Now that New York’s numbers have stabilized, we’re returning the favor across the country, and I am glad to be able to help the great city of Houston establish two testing sites in vulnerable communities.”
The sites are located at Fallbrook Church (12,512 Walters Rd.), which opened today, and at Higher Dimension Church (9800 Club Creek Dr.), which will open tomorrow.
In addition, Cuomo’s support will go toward helping the Houston Health Department’s major testing sites at Butler and Del Mar Stadiums, as well as 16 affiliated sites.
“Houston is grateful for the support from Governor Cuomo and the people of New York. I commend the governor and his people for their concentrated efforts in slowing down the spread of this virus,” Turner said in a statement. “We value the partnership and thank them for sending a team and supplies to open two testing sites. Testing is critically important in Houston, especially in the Black and Hispanic communities that have been hit hardest by COVID-19.”
Houston is the latest city to receive help from New York. Earlier this week, Cuomo sent testing and contact tracing teams to Atlanta, Georgia, and remdesivir to Florida.
The National Academies of Sciences, Engineering, and Medicine urge school districts to prioritize reopening
The National Academies of Sciences, Engineering, and Medicine is recommending school districts reopen schools full time for grades K-5 and for students with special needs.
The academies published a new report yesterday, encouraging schools to consider the educational risks of not providing in-person instruction. By shutting down schools and delaying students’ education, the pandemic could have detrimental, long-term academic effects on students—particularly young children—if they are unable to keep up with their lessons.
In addition, delaying the opening schools will impact families that rely on child care, school services and meals for support.
“This pandemic has laid bare the deep, enduring inequities that afflict our country and our schools,” said Enriqueta Bond, Ph.D., chair of the committee that authored the report. “Many of the communities hardest hit by the virus are also home to schools with the least resources and the greatest challenges. Education leaders need to be careful when making the decision to reopen to not exacerbate these inequities.”
Russian hackers target coronavirus vaccine research
U.S., British and Canadian security officials reported today that a Russian hacking collective, known as APT29, has been attempting to steal coronavirus vaccine research and intellectual property.
The hacking group, which also refers to itself as “the Duke” and “Cozy Bear,” is linked to Russian intelligence and was responsible for the 2016 hacking of the Democratic National Committee.
Using malware code known as “WellMess” and “WellMail,” the hackers sent fake emails to American, British and Canadian health organizations and labs to gain access to vaccine research, data and medical supply chain information.
Officials did not release the identities of the targets or confirm whether or not the hackers were successful in their hacking attempts. Considering the global race to develop a vaccine, many countries have already forewarned research facilities, hospitals and pharmaceutical companies to ramp up cybersecurity to protect their intellectual data.
Hydroxychloroquine ineffective in reducing COVID-19 symptoms
Clinical trial results of hydroxychloroquine failed to show any substantial effect in reducing the symptoms in patients with early, mild cases of COVID-19, according to a new study published today in the Annals of Internal Medicine.
The randomized trial, conducted by researchers from the University of Minnesota, investigated whether or not a course of hydroxychloroquine administered in the first four days of a patient’s symptoms would effectively minimize the severity and duration of symptoms and prevent hospitalization.
Participants received 800 mg of oral hydroxychloroquine once, followed by 600 mg six to eight hours later, then 600mg daily for 4 more days.
At the end of the study, however, researchers found no difference between hydroxychloroquine and the placebo in any of the 423 patients whom they were able to study. After two weeks, 24 percent of those receiving hydroxychloroquine and 30 percent of those who received the placebo continued to have symptoms. —Shanley Pierce
UPDATE | July 15, 2020, 2:45 p.m.: The first published data on Moderna’s highly anticipated COVID-19 vaccine showed encouraging outcomes.
Results from the first-in-human phase 1 clinical trial, which were published yesterday in the New England Journal of Medicine, indicated that the candidate vaccine, mRNA-1273, induced an immune response against SARS-CoV-2 in all 45 participants of the study.
mRNA-1273 has been a main target for vaccine development for COVID-19. It encodes the SARS-CoV-2 spike glycoprotein, which the virus uses to attach to a surface protein on human cells—called ACE2—and gain entry into the host cell to replicate the viral RNA into new copies.
After participants received the vaccine, which was administered in two doses four weeks apart, all of them were reported to have produced neutralizing antibodies against SARS-CoV-2 without serious toxicity or adverse side effects. The vaccine was most effective using a 100-microgram dose.
While these findings are promising, further tests are required to determine whether or not the antibodies will prevent infections in the future and how long that protection will last.
Currently, a phase 2 trial of Moderna’s vaccine—50-microgram and 100-microgram dosages—is being tested in 600 healthy adults. The phase 3 trials, testing the 100-microgram dose, are slated to begin this summer.
Hospitals directed to stop reporting coronavirus data to CDC
The U.S. Department of Health and Human Services (DHHS) has ordered hospitals to stop sending COVID-19 patient data to the Centers for Disease Control and Prevention (CDC), effective today.
All daily reports regarding COVID-19 patients, available ventilators and capacity and other information will be sent to DHHS, instead of the CDC’s National Healthcare Safety Network site. The shift in responsibility has raised concerns about data transparency.
The order, which was issued on Monday, requires data to be submitted through the federal TeleTracking portal. This system was previously used by hospitals to determine which states received allocated shares of remdesivir.
The Texas Department of State Health Services urged hospitals to continue reporting to the state and to the federal government.
New case studies drive CDC to urge Americans to wear face coverings
After reviewing two case studies, the CDC affirmed that wearing cloth face coverings is effective in controlling the community spread of the virus.
“We are not defenseless against COVID-19,” CDC director Robert R. Redfield, M.D., said in a press release. “Cloth face coverings are one of the most powerful weapons we have to slow and stop the spread of the virus—particularly when used universally within a community setting. All Americans have a responsibility to protect themselves, their families, and their communities.”
One of the studies showed that a universal masking policy effectively reduced SARS-CoV-2 transmission at a Boston hospital health care system, while the other study found that double-layer masks prevented two COVID-19-positive hair stylists at a Missouri salon from transmitting the virus to their clients.
The two stylists continued to see 139 clients—one for four days and the second for eight days—after developing respiratory symptoms due to virus. Nearly all the clients wore a face covering of some form. Among the 67 clients who volunteered to be tested for the study, none of them tested positive for SARS-CoV-2—reinforcing the importance and efficacy of adhering to face covering policies. — Shanley Pierce
UPDATE | July 14, 2020, 1:25 p.m.: Yesterday, Texas reported a small drop in hospitalizations related to COVID-19 across the state.
In the Texas Medical Center, the ICU bed configuration and staffing under Phase 1, which is the non-pandemic configuration, is currently full, and the TMC is six percent into the Phase 2 plans for intensive care. At the current growth rate, the TMC predicts that they will not move into Phase 3 ICU capacity within two weeks. Comprehensive updates about ICU capacity and other growth trends related to COVID-19 in the Texas Medical Center can be accessed at tmc.edu.
Fort Bend ISD announced that it will start the fall school year online, with no in-person instruction or extra-curricular activities. In national news, the Los Angeles and San Diego school districts announced that they would be online-only for the entire fall semester. Yesterday also brought another partial shutdown in California, with the governor closing indoor activities including restaurants, movie theaters and bars as COVID-19 cases continue to rise at alarming rates throughout that state.
A new contact-tracing study has linked 43 new cases of COVID-19, as well as 68 exposed close contacts, to one large house party in Michigan that took place in early July. The study found that most of the individuals affected were between the ages of 15 and 25.
Another study from Catawba County in North Carolina linked a family gathering to 41 new coronavirus cases over 16 days. The public health department created a striking infographic to illustrate how easily the virus spreads from person-to-person interaction.
In innovation news, researchers from the University of Houston were part of a team that created an air filter that can effectively “catch and kill” the SARS-CoV-2 virus. The filter, described in a study published July 7 in the journal Materials Today Physics, is made from nickel foam and heated to 200 degrees Celsius. During tests at the Galveston National Laboratory, the filter killed 99.8 percent of the virus in a single pass. The designers believe the filter could be used in indoor spaces to improve the safety of essential workers and the general public.
Mayor Sylvester Turner has invited the public to a virtual town hall meeting focused on mental health, healing and wellness amid the COVID-19 pandemic. Hosted by the Houston Health Equity Response (H.E.R.) taskforce’s Faith-Based Subcommittee, the forum will take place on Friday, July 24, from 6 to 7:30 p.m. Registration is required.
Also notable is news that city officials from San Antonio have confirmed the presence of refrigerator trucks “on standby” should they be needed for the rising number of COVID-19 deaths in the area. The trucks would be used to take bodies from hospitals until they could be transferred to a morgue or funeral home. — Alexandra Becker
UPDATE | July 13, 2020, 8 p.m.: Houston Mayor Sylvester Turner has asked Gov. Greg Abbott for the right to “reset” the Bayou City in hopes of gaining control of the surging COVID-19 virus this month. Harris County Judge Lina Hidalgo also has called for similar authority.
In a news conference today, Turner said he had not spoken to the governor personally about his request for a “two-week shutdown,” which would include a stay-at-home order and a return to Phase 1 for businesses, which is 25 percent maximum occupancy.
“I don’t think it’s going to be enough to slow down the progression of this virus in time to keep our systems from being overwhelmed. I think we are going to have to do some additional things,” Turner said. “I am looking at the numbers from the hospitals every single morning and I do know we are continuing to creep up.”
On Monday, Houston crossed 30,000 confirmed total infections with 30,965. The mayor also reported 1,544 new cases. The goal to adequately track the virus is 300 or fewer daily cases over a seven-day period, Turner said.
The city also added eight confirmed deaths for 277 total.
“COVID-19 is a virus that continues to run rampant in our city,” the mayor said. “What we do today and over the next few weeks is critical to getting this virus back to some degree of control and a virus we can manage.”
Gaining control means at least a 90 percent compliance on masks and face coverings, Turner said. His message was amplified by new animation with Houston rapper Trae tha Truth for the MaskUp! campaign.
As we head into a new week, let’s all be like @TRAEABN and his chain.
Please #maskuphou and continue to #socialdistance. ??? pic.twitter.com/eHLQOJZp21
— Sylvester Turner (@SylvesterTurner) July 13, 2020
Houston Rockets star Russell Westbrook has tested positive for COVID-19 and shared messages on social media that echoed the mayor’s Mask Up! campaign.
Testing, contact tracing and hospital capacity continue to be “strained,” the mayor said.
Turner added that he wants the economy to remain open and “for people to be able to hang on to their jobs.” He also said that what we do in July will determine whether the schools will be able to open in August.
Turner also encouraged those who can to work remotely to do so and asked that everyone avoid large gatherings including house parties, so that “we don’t overwhelm our health care delivery system such that if people need a bed, there will be a bed for them—and not just for COVID-19, but if they are suffering from strokes or diabetes or any other illness.”
The positivity rate is now 26.8 percent for COVID-19 tests administered in the city, said David Persse, M.D., the city’s health authority. At the end of June, the positivity rate was 25.2 percent. In March, the rate was 14.7 percent, he said.
A U.S. Army Urban Augmentation Medical Task Force (UAMTF) arrived in Houston today. The team is expected to establish a 30-to-50 bed hospital in an empty wing at the United Memorial Medical Center in north Houston to “lighten the loads of other hospitals,” Persse said at the news conference.
Also, a “medical resort” in the Willowbrook area—a vacated nursing home—will serve as a respite for patients “who have been hospitalized and are improving, but just aren’t quite ready to go home,” Persse said.
Rice University was featured today in The New York Times for its plan to build nine outdoor classrooms this summer.
“Five are open-sided circus tents that the university is buying, and another four are semi-permanent structures that workers are building in an open field near dorms, Kevin Kirby, Rice’s vice president for administration, told me. Students and professors will decorate the spaces with murals and video projections,” the David Leonhardt column said.
Finally, the Texas Supreme Court denied the state GOP’s appeal to continue with its in-person convention in downtown Houston, which was scheduled to begin today. This is the third court to turn down a legal request by the Republican Party of Texas following the city’s cancellation of the meeting contract because of COVID-19. The party plans to convene online, the organization announced late Monday. — Cindy George
UPDATE | July 10, 2020, 3 p.m.: Texas is reporting a 15.5 percent positivity rate for COVID-19, while Houston is reporting 20,753 active cases and 250 deaths.
Due to high temperatures today, Harris County Public Health closed COVID-19 testing sites at noon. Those who had appointments today can bring their code on Saturday to get tested.
A recent tweet offers the most recent combined COVID-19 data from Harris County and Houston:
• This week, 239 scientists around the world sent an open letter to the World Health Organization (WHO) to “recognize the potential for airborne spread of COVID-19.”
Currently, WHO recommendations are based on the assumption that the disease is carried in larger respiratory droplets that contaminate objects and surfaces.
While WHO promotes hand washing, social distancing and other actions to quell the spread of the illness, these guidelines “are insufficient to provide protection from virus-carrying respiratory microdroplets released into the air by infected people,” the scientists argue. Microdroplets, also known as aerosols, can linger in the air after people have departed, the scientists maintain, and some COVID-19 hotspots and outbreaks are explainable only by airborne transmission of the disease.
The 200-plus scientists are recommending that WHO offer clearer control measures to fight the airborne spread COVID-19 that include providing effective ventilation in public buildings and supplementing general ventilation with high efficiency air filtration and ultraviolet lights. In some cases, opening doors and windows can increase air flow, they note.
“It is understood that there is not as yet universal acceptance of airborne transmission of SARS-CoV2; but in our collective assessment there is more than enough supporting evidence so that the precautionary principle should apply,” the scientists write. “In order to control the pandemic, pending the availability of a vaccine, all routes of transmission must be interrupted.”
WHO acknowledged the possibility of airborne transmission of COVID-19 in a news release posted on Thursday:
“There have been reported outbreaks of COVID-19 in some closed settings, such as restaurants, nightclubs, places of worship or places of work where people may be shouting, talking, or singing,” the release states. “In these outbreaks, aerosol transmission, particularly in these indoor locations where there are crowded and inadequately ventilated spaces where infected persons spend long periods of time with others, cannot be ruled out. More studies are urgently needed to investigate such instances and assess their significance for transmission of COVID-19.”
• Black medical professionals are speaking up about systemic racism experienced throughout their careers. In an essay posted online today in the New England Journal of Medicine, Vanessa Grubbs, M.D., who is affiliated with the University of California, San Francisco, outlines ways for academic medical institutions to create diversity, equity and inclusion.
“At the trainee level, real action is accepting candidates that may not fit all the criteria that favor people who’ve always been highly favored,” Grubbs notes. “Letters of recommendation are often tinged with racial bias, and test scores are biased toward those who can afford prep courses.”
At the faculty level, she continues, real action means offering faculty and leadership positions to non-prototypical candidates. “As the only Black member of division-chief search committees,” Grubbs notes, “I often heard colleagues remark that the Black candidate’s CV was thinner than the White man’s — fewer manuscripts, leadership positions, and grants — without acknowledging that the White man had been groomed, sponsored, and uplifted by people who looked like him throughout his 400-year head start.”
In order to retain Black faculty, she concludes, institutional leadership must “believe, validate, and act on Black people’s experiences of racism.” —Maggie Galehouse
UPDATE | July 9, 2020, 9 p.m.: People are dying at home from COVID-19 before help arrives, according to information from Houston’s health authority and the city fire chief as well as a new ProPublic/NBC News analysis.
“There’s a distinct possibility that there is an undercounting of the COVID-related deaths. In order for a death to be recorded as COVID-related, the death certificate needs to have something from the physician indicating a COVID-related illness,” David Persse, M.D., Houston’s health authority, said today at Houston Mayor Sylvester Turner’s news conference.
The Houston Fire Department has been finding people not breathing and not having a pulse. Some are DOA, dead on arrival, while others can be resuscitated.
Three days ago, HFD had 18 DOA calls—the most in one day all year, said Houston Fire Department Chief Samuel Peña.
“They’re having critical medical emergencies and there is nothing we can do by the time we get to the scene,” Peña said. “Do not wait to call 911 if you are having cardiac issues, respiratory issues, signs and symptoms of a stroke.”
The fire chief noted that fewer firefighters are in quarantine, but the agency is running at a heightened 1,100-plus calls a day.
A new ProPublica/NBC News report reveals that many COVID-related deaths in the Bayou City are people who never receive medical care, but end up at the morgue where their infections are counted among the COVID-19 deaths.
“In Houston, one of the nation’s fastest-growing coronavirus hot spots, more residents are dying before they can make it to a hospital. Medical examiner data shows that an increasing number of these deaths are the result of COVID-19,” the story said. “In the Houston area, the trend can be seen in autopsies performed by the Harris County Institute of Forensic Sciences. In May, among people who had died unexpectedly at home, the county medical examiner attributed just six deaths to COVID-19. In June, the number jumped to 19, with most of those cases coming in the second half of the month, coinciding with a surge in the number of confirmed coronavirus cases locally. Because the medical examiner only performs autopsies in a fraction of cases, these numbers are not comprehensive.
More broadly, Houston emergency responders have also seen an increase in deaths during cardiac arrest calls.”
Houston Mayor Sylvester Turner wore a Census 2020 mask today at his news conference to emphasize the continuing need for more people to respond to the decennial count.
“With all of the federal dollars and resources that we need to combat the pandemic, quite frankly, it’s all tied to the Census,” he said.
Houston’s response—about 52.5 percent of the city’s estimated 2.32 million residents—falls below the average national response, which is above 60 percent, according to the most recent data.
“I want to encourage people to take the time to respond to the census—2020Census.gov—online. Nine questions. It doesn’t take very long at all,” the mayor said. “For each person who goes unaccounted, Houston loses about $1,500 … per year in government funds for the next 10 years. So, even a 1 percent undercount could cost the City of Houston $250 million in federal dollars. … We need that money for education, housing, health care—and representation for the Census is very important when you are trying to fight COVID-19.”
The Houston Health Department is reporting 412 new COVID-19 cases, bringing the city’s total to 26,012, with five new deaths for 250 fatalities in all. The new deaths include a Hispanic male in his 30s with underlying health conditions.
“The COVID-19 virus in the city, and quite frankly, in the state is out of control. What we do today and over the next few weeks is critical to getting this virus back in a manageable state,” Turner said, adding that the goal is to bring the number of new cases reported daily in the city to 300 or fewer. “That makes it then much more practical for us to engage with our contact tracing.”
New free testing sites will be opening in Second Ward and the Alief area soon.
Additionally, the ongoing saga of the Republican Party of Texas v. Turner—tension over a state GOP convention scheduled next week in Houston that was canceled Wednesday by the city because of the coronavirus transmission risk—became a lawsuit Thursday. Later in the day, state District Judge Larry Weiman denied the party’s request to block the city from canceling the contract. In a statement, the party announced its intention to “proceed in filing its appeal directly to the Texas Supreme Court given the time sensitivity of the matter as the Convention was scheduled to begin its committee meetings on Monday at the George R. Brown Convention Center.” — Cindy George
UPDATE | July 8, 2020, 4:15 p.m.: After a record single-day report of more than 60,000 new coronavirus cases, the United States now has exceeded the 3 million mark, according to the Johns Hopkins University COVID-19 tracker.
Republican Party of Texas in-person convention canceled
The Republican Party of Texas convention has now been canceled.
This afternoon, Turner instructed Houston First, the city’s convention bureau, to exercise its contractual right to cancel the event due to the pandemic. The organization issued a letter, which was signed by its president and chairman, to the State Republican Executive Committee, canceling the convention.
“These are some very serious times and the public safety of people attending the convention, the employees, the family members and the people in the city of Houston—their public health concerns are first and foremost paramount,” Turner said Wednesday during a press conference.
After Turner asked the city attorney and Houston First to review the contract this morning, the mayor announced that they were able to identify a provision that would allow them to cancel the event.
Section 12 of the terms and conditions portion of the license agreement states that either party may terminate the agreement or suspend its obligations due to force majeure to the extent that such occurrence is beyond a reasonable control of the party whose performance is affected.
The term “force majeure” was defined in the contract to include epidemics in the city of Houston, as well as emergency governmental declarations and other occurrences of similar nature, Turner said.
The meeting was scheduled to be held July 16 to July 18 at the George R. Brown Convention Center in downtown Houston and expected to host approximately 6,000 guests.
Trump formally withdraws from WHO
The Trump administration notified Congress and the United Nations that the U.S. would be withdrawing from the World Health Organization (WHO) effective July 6, 2021.
President Trump issued a letter in May that stated he would be cutting ties with the WHO after arguing the agency mismanaged its response to the COVID-19 pandemic, claiming it “ignored credible reports of the virus,” “chose not to share any critical information” and “made claims about the coronavirus that were either grossly inaccurate or misleading.”
As the top contributor to the WHO, making up 15 percent of the agency’s total funding and providing $893 million for 2018 and 2019, the withdrawal of the U.S. would significantly impact global programs, primarily polio eradication and increasing access to essential health and nutrition services.
Considering Trump’s decision to remove U.S. involvement from the WHO doesn’t start for another year, his plan depends on the results of the 2020 presidential election. If Trump loses the election to presumptive Democratic nominee Joe Biden, the former U.S. vice president could overturn that order and has stated that maintain the nation’s relationship with the WHO.
“Americans are safer when America is engaged in strengthening global health. On my first day as President, I will rejoin the WHO and restore our leadership on the world stage,” Biden tweeted Tuesday.
First disinfectant sprays approved by the EPA to kill COVID-19 virus
The Environmental Protection Agency (EPA) approved two disinfectant products manufactured by Lysol to safely and effectively eliminate SARS-CoV-2, the virus that causes COVID-19.
Having been tested directly against SARS-CoV-2, the two common household products—Lysol Disinfectant Spray and Lysol Disinfectant Max Cover Mist— are the first surface disinfectants approved by the agency. The sprays, which use quaternary ammonium and ethyl alcohol as the main ingredients, can effectively kill the novel coronavirus on hard nonporous surfaces in two minutes.
According to the EPA, manufacturers cannot legally claim that a product can eliminate a pathogen, including SARS-CoV-2, before receiving the agency’s approval and authorization to be added to its “Disinfectants for Use Against SARS-CoV-2” list, also known as List N, which includes more than 430 products.
All products on List N must meet the agency’s criteria to demonstrate effectiveness against SARS-CoV-2, viruses that are harder to kill than SARS-CoV-2 or another type of human coronavirus similar to SARS-CoV-2. — Shanley Pierce
UPDATE | July 7, 2020, noon: The United States is set to exceed 3 million cases of COVID-19, according to a STAT News tracker, which draws data sets from more than 15 sources. The 3 million mark comes nearly one month after the nation’s case count exceeded 2 million. Meanwhile, Texas is reporting a 13.5 percent positivity rate as of July 5, and the City of Houston reports 19,343 active cases, with 239 deaths.
The New York Times reported this morning that the United States plans to pay $1.6 billion for the development of 100 million doses of a vaccine for COVID-19 disease. The deal, made by the Trump administration with Maryland-based vaccine development company Novavax, is part of the administration’s “Operation Warp Speed”—which aims to make treatments for COVID-19 available to the American public as soon as possible. According to the newpaper’s report, Novavax has never before brought a product to market.
The Texas Medical Association recently released a chart rating activities based on their risk for contracting COVID-19 disease. Opening the mail ranked least risky while activities such as going to a bar, attending a religious service with more than 500 worshipers and going to a sports stadium or large concert were among the riskiest behaviors. Moderate risk activities included backyard barbecues, sending kids to camp or day care and going to the beach.
The American Academy of Pediatrics (AAP) has released a comprehensive recommendation regarding the re-opening of schools. The guidance, which includes physical distancing measures and specific recommendations for different grade levels and other considerations, states that, “the AAP strongly advocates that all policy considerations for the coming school year should start with a goal of having students physically present in school.” The guidance goes on to state that the importance of in-person learning is well documented, and that the negative impacts on children as a result of the spring 2020 school closures is already evident, including learning loss and social isolation along with resulting emotional and health issues. The AAP also cites ongoing evidence that young children are not as susceptible as adults to SARS-CoV-2, the virus that causes COVID-19.
Houston Mayor Sylvester Turner announced details of this year’s Beat the Heat program. Sponsored by Reliant, the program—in its 15th consecutive year—was created to help area residents stay cool during Houston’s hot summer months. This year’s Beat the Heat has been reimagined to adhere to social distancing guidelines recommended by the CDC, and will focus on providing seniors and vulnerable residents assistance through portable air conditioning units and care packages. Reliant has donated $80,000 to the Houston Health Department and the public service organization Precinct2gether to help fund this initiative and will also offer bill payment assistance and flexible payment options for qualified customers. The Beat the Heat program also has measures in place to open emergency cooling centers as necessary, with strict infection control practices in place.
Also announced today: The Texas State Fair, held each fall in Dallas, will be canceled this year due to concerns about the pandemic. This is the first time the event has been called off since World War II. —Alexandra Becker
UPDATE | July 6, 2020, 4:30 p.m.: The Houston Health Department has launched a three-week emergency outreach program to help curb the spread of COVID-19 in the Hispanic community, which is heavily affected by the disease.
Better Together/Todos Juntos Mejor aims to educate Hispanics about the best ways to prevent the spread of COVID-19 and direct people to helpful resources throughout the city.
“The Latino community makes up 42 percent of the Houston cases in which our epidemiologists were able to verify race and ethnicity,” Porfirio Villarreal, public information officer at the health department, said in a news release. “Our goal with ‘Better Together’ is to provide easy access to potentially lifesaving information with a click, visit or call.”
• Houston Mayor Sylvester Turner and other city leaders are sending a letter to the executive director of the Republican Party of Texas to ask that the in-person GOP convention scheduled for July 16-18 at the George R. Brown Convention Center be cancelled and replaced by a virtual meeting, in light of the rise in COVID-19 cases in the city.
“I believe this is the responsible action to take,” Turner said in a news conference Monday afternoon. “Hosting an indoor convention at this time in Houston is a bad idea. I am going to call on the [event] sponsors to join in with us in asking the State Republican Executive Committee to cancel their plans.”
• A federal assessment team has arrived in Houston to help determine how the U.S. government could help the city respond to a surge in COVID-19 cases across the city, said Houston health authority David Persse, M.D., in Monday’s news conference.
“We’re getting help from outside,” Persse said, adding that the state has brought in about 120 nurses to support expanding operations and provide relief for local health workers.
• The Houston Health Department and Texas Division of Emergency Management (TDEM) have opened four free drive-thru COVID-19 testing sites this week, operating today through Saturday, July 11, at the following locations:
- Eden Event Center, 7450 N. Wayside Drive
- NRG Park, Green Lot, 1 Reliant Park
- HCC – Northeast Campus, 555 Community College Drive
- HCC – South Campus, 1990 Airport Blvd.
TDEM requires appointments, which can be made by visiting txcovidtest.org. Click here for a complete list of free testing sites in the area this week.
• According to Harris County Public Health’s COVID-19 dashboard, there are currently 24,134 active cases of COVID-19 in Harris County and the City of Houston combined, while the death toll has risen to 400. — Maggie Galehouse
UPDATE | July 2, 2020, 4 p.m.: Surgeon General Jerome Adams, M.D., shared a video message in anticipation of the Fourth of July weekend. He asked people to protect themselves and their loved ones by doing a few simple things:
“Even though not all of us risk a severe case of coronavirus, we all risk getting it and spreading it to others—maybe without even realizing that we’re sick,” Adams said.
He reminded Americans to wash their hands frequently, stay 6 feet from others and wear a face covering.
• At an afternoon press conference, Houston Mayor Sylvester Turner made several recommendations to blunt the progression of COVID-19 in Houston over the next three weeks.
Turner is asking for voluntary compliance of these recommendations because he does not have the authority to mandate guidelines.
He asked each resident to wear a mask in the presence of other people, both inside and outside of businesses; maintain social distancing in the workplace and, if that is impossible, work remotely; and to reduce social gatherings to no more than 10 people, especially as the city heads into the July 4th weekend.
He also asked businesses to reduce their occupancy from 50 percent to 25 percent and requested that faith-based groups resume or continue virtual worship.
Houston health authority David Persse, M.D., noted that younger people are increasingly vulnerable to COVID-19.
“Fifteen percent of those admitted to the hospital are under 50,” Persse said. “Thirty percent are under 60.”
The city’s Fourth of July celebration will be virtual this year and city leaders ask that individuals enjoy the program on television and from their homes. The Shell Freedom Over Texas celebration will feature the Houston Symphony Orchestra backing several artists, live, including Trae tha Truth, Bun B and Mariachi Imperial de America.
The live fireworks show has been reconfigured to provide a more elevated display—800 feet, as opposed to 450 feet—so more people will be able to see the pyrotechnics from a greater distance.
The celebration will air on ABC13 Houston from 7 to 10 p.m. Saturday.
• Harris County and the City of Houston are reporting 21,462 active cases of COVID-19 today, while the death toll has risen to 384, according to Harris County Public Health’s COVID-19 dashboard. The county’s threat level remains at Level 1, or “severe.”
• Gov. Greg Abbott on Thursday afternoon issued an order that requires all Texans to wear a mask or face covering in public spaces. The order applies to counties with 20 or more cases of COVID-19, which includes Harris County as well as other Houston-area jurisdictions including Fort Bend, Montgomery, Brazoria, Waller, Chambers, Liberty and Galveston counties.
• The Centers for Disease Control and Prevention (CDC) reports 2,679,230 cases of COVID-19 across the country today, an increase of 54,357 cases since yesterday. Total COVID-19 related deaths across the country have reached 128,024, an increase of 725 since yesterday.
• STAT News reports that some experts believe using temperature checks to gauge whether individuals have COVID-19 is unreliable and that smell tests would be more accurate, since a loss of smell—anosmia—is an earlier symptom of the disease than fever. The story cites a recent Mayo Clinic study that found “Covid-19 patients were 27 times more likely than others to have lost their sense of smell. But they were only 2.6 times more likely to have fever or chills, suggesting that anosmia produces a clearer signal and may therefore be a better Covid-catching net than fever.” — Maggie Galehouse
UPDATE | July 1, 2020, 3:50 p.m.: According to Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases, the United States is projected to see 100,000 new cases of COVID-19 each day if current trends continue.
During a hearing before the Senate Health, Education, Labor and Pensions Committee yesterday, the country’s leading infectious disease expert warned that the number of new COVID-19 cases is on the rise.
Currently, there are more than 40,000 new cases each day, forcing states that aggressively pushed forward with reopening—including Texas—to pull back.
“Clearly we are not in total control right now,” Fauci said. “It is going to be very disturbing, I will guarantee you that, because when you have an outbreak in one part of the country, even though in other parts of the country they’re doing well, they are vulnerable.”
New housing initiative to assist increasing homelessness during the coronavirus pandemic
Houston Mayor Sylvester Turner and Harris County Judge Lina Hidalgo announced today a new permanent housing initiative to assist those experiencing homelessness
In partnership with the Coalition for the Homeless, the $65 million COVID-19 homeless housing program will permanently house 5,000 individuals in less than two years.
“This is the largest, most ambitious homeless initiative in the history of the city or county, but it’s not about the amount of funding, rather the number of lives that the initiative will transform—more than doubling the number of homeless individuals that are annually housed,” Turner said during his news conference this afternoon.
Because of underlying health conditions and a lack of access to health care, people experiencing homelessness are especially susceptible to the coronavirus and are at a higher rate of experiencing severe symptoms.
“This is an emergency response to an infectious disease, but one that will have a permanent impact by significantly decreasing our homeless population,” Turner added. “The situation is only compounded by the prospect of thousands falling into homelessness because of the economic impact of the coronavirus. We are responding now to protect the health of at-risk homeless individuals, prevent potential communal spread and assist those forced into homeless by COVID-19.”
According to city reports, the annual homeless count reveals that after substantial investment from the city and county since 2012, the unhoused population was reduced by 55 percent reduction. However, over the past three years, the size of the homeless population has remained steady.
“This is probably not going to be a one-time solution,” Hidalgo said. “We’re going to have to continue with this work, continue with these investments, but oftentimes the hardest thing is just to change that strategy, while identifying the most strategic and smartest way to address a problem. I think we’re finding it and we’re finding that we get there together.” — Shanley Pierce
UPDATE | June 30, 2020, 11:25 a.m.: Two new studies published in the New England Journal of Medicine describe hundreds of cases of MIS-C (Multisystem Inflammatory Syndrome in Children) as a side effect of COVID-19. One of the studies, led by Boston Children’s Hospital and based on targeted surveillance in pediatric health centers across the United States, reported that 80 percent of the children who developed the condition required intensive care while 20 percent required mechanical ventilation; 88 percent were hospitalized and four children died. The other study, based in New York state, also reported that 80 percent of the patients studied were admitted to an intensive care unit with two deaths.
“Multisystem inflammatory syndrome in children associated with SARS-CoV-2 led to serious and life-threatening illness in previously healthy children and adolescents,” the Boston Children’s concluded.
Gilead Sciences, the biopharmaceutical company behind the drug remdesivir—a promising experimental treatment for COVID-19—has announced that it will charge $3,120 for a full course of the five-day therapy for insured patients in the U.S. It is unclear how much uninsured patients would be charged, but the company stated a discounted price of $2,340 for developed countries besides the U.S.
The pricing has been met with mixed reactions. Many have voiced concerned about the drug maker realizing a profit during this public health crisis. In response to the criticism, Daniel O’Day, the chairman and CEO of Gilead Sciences, wrote an open letter explaining the prices, stating that, “there is no playbook for how to price a new medicine in a pandemic,” and that the company is “aware of the significant responsibility that comes with pricing remdesivir, and the need to be transparent on our decision.”
Harris County Judge Lina Hidalgo is currently following CDC guidelines and quarantining at home after being in contact last week with an individual who later tested positive for COVID-19. She has shown no symptoms and wrote in a tweet yesterday that she is “feeling great” and was tested earlier that morning.
“We’ll update folks as soon as the results come back. Please remember to stay home. This uncontrolled growth in hospitalizations will not flatten itself,” the tweet read.
According to Harris County Public Health’s COVID-19 dashboard, there are currently 19,955 active cases of COVID-19 in Harris County and the City of Houston combined, and the death toll has risen to 376. Harris County’s threat level remains at Level 1, or “severe,” indicating that “outbreaks are present and worsening and that testing and contact tracing capacity is strained or exceeded,” according to the county’s website. All residents are encouraged to minimize contact with others and avoid leaving home except for essentials. — Alexandra Becker
UPDATE | June 29, 2020, 7 p.m.: Mayor Sylvester Turner is at his wit’s end.
COVID-19 cases and deaths continue to increase, Houston hospitals are filling up, a larger share of inpatients are under 40 and the percentage of positive tests have increased.
Despite a governor’s order closing bars and clubs as of noon Friday, some of those Houston businesses were packed this weekend amid the global health pandemic hitting Texas hard.
“This is real. People are dying. People are getting sick. People are going to the hospital. People are in ICU beds and people who are asymptomatic are infecting their loved ones,” the mayor said at an afternoon news conference. “So, it just doesn’t make sense and, quite frankly, I have lost patience.”
Turner has inaugurated his COVID-19 “Wall of Shame” with three businesses: Spire, Pour Behavior and Prospect Park Sports Bar & Kitchen.
“People know you shouldn’t be in a crowded capacity, shoulder-to-shoulder, not wearing a mask; that simply is a formula to be infected,” the mayor said. “If you see that a place shouldn’t be open, but it is open, you shouldn’t be walking into the doors. And then if you are going in a place that is crowded where you can’t engage in social distancing, people don’t have on their masks, then you should turn around and walk out.”
The city’s largest drive-thru testing sites at Delmar Stadium and Butler Stadium reached capacity before noon Monday. The city will be increasing daily testing capability at both locations from 500 to 650 per site while working to expand testing elsewhere.
According to Turner, the city’s positive tests were around 3% in April, but have increased to above 13%.
“My fear is that we will see that number to continue to rise,” said David Persse, M.D., the city’s health authority. “What that reflects, of course, is not that complicated. It’s that there is more virus in the community than previously expected.”
Houston Fire Chief Samuel Peña offered another perspective on hospital capacity and the amount of illness in the community.
“Call volume has increased about 30 percent” in two months, he said, adding that crews are responding primarily to cases of respiratory difficulty, a key symptom of COVID-19. “Over the last three weeks, we’ve had over 560 instances where ambulances are at the hospital waiting to give, report and transfer the patient for over an hour. That has an impact on our ability to be in service, on the steet and ready to respond to the next call.”
The HFD occupancy task force also responded to more than 300 complaints about overcrowded bars, clubs and restaurants this week, Peña added. — Cindy George
UPDATE | June 26, 2020, 4 p.m.: At noon today, Harris County raised its COVID-19 Threat System to Level 1, signifying severe and uncontrolled levels of COVID-19 across the county. Outbreaks are worsening and the county’s ability to perform testing and contact tracing is strained. Residents are encouraged to stay home and work safe.
“At this level, residents take action to minimize contact with others wherever possible and avoid leaving home except for the most essential needs, like going to the grocery store for food and medicine,” the county website explained.
At a late morning press conference, Harris County Judge Lina Hidalgo spoke about the current circumstances.
“Today, we find ourselves careening toward a catastrophic and unsustainable situation,” she said. “Our current hospitalization rate is on pace to overwhelm the hospitals in the near future. … It is incumbent on all of us to buckle down and act.”
Although there is space in hospital surge capacity right now, she said, that space could run out in a matter of weeks.
Hidalgo compared the coronavirus pandemic to “an invisible hurricane,” during which Houstonians should show the same compassion and care towards neighbors and fellow citizens as they did during the storms and floods that have ravaged the city.
“Our hospitals … are using 100 percent of their base operational capacity right now,” she said. “Our situation is far worse today than when we issued the first Stay Home order in Harris County.”
Although Hidalgo does not have the authority to issue a Stay Home Work Safe Order, as she did earlier in the pandemic, she is issuing an advisory that mirrors the initial order exactly, she said.
• Today, Texas Gov. Greg Abbott dialed back the reopening of the Texas economy with an executive order that limits some businesses and services in order to stem the rapid spread of COVID 19.
The following updates are included in the order:
- All bars and similar establishments that receive more than 51% of their gross receipts from the sale of alcoholic beverages are required to close at noon today. These businesses may remain open for delivery and take-out, including for alcoholic beverages, as authorized by the Texas Alcoholic Beverage Commission.
- Restaurants may remain open for dine-in service, but at a capacity not to exceed 50 percent of total listed indoor occupancy, beginning Monday, June 29, 2020.
- Rafting and tubing businesses must close.
- Outdoor gatherings of 100 or more people must be approved by local governments, with certain exceptions.
• Houston Mayor Sylvester Turner joined COVID-19 recovery czar Marvin Odum, local health authority David Persse, M.D., and other city officials in a press conference to discuss the spike in COVID-19 cases across the city.
Houston health authority David Persse, M.D., discusses COVID-19 at a June 26, 2020 press conference.
Houston saw 879 new cases of COVID-19 today, bringing the current total to 1,856.
“The case load is the highest it has been at any point since this whole thing started,” Turner said.
The city is also reporting 8 new deaths, bringing the total to 216, he added. Of that 216, 63 are associated with nursing homes and 3 with Harris County Jail.
Odum, who spoke briefly, said: “Wear a mask, stay 6 feet apart and keep your hands clean. … It all hinges on Houstonians doing the right thing. You need to demand this of yourself and you need to demand it of everyone else.”
• The Centers for Disease Control and Prevention (CDC) on June 25 updated and expanded its list of who is at increased risk for getting severely ill from COVID-19.
While older individuals and people with underlying medical conditions are still at great risk, the CDC has removed the age threshold for older adults and now warns that risk increases as people age and that those at increased risk for severe illness are not simply individuals over age 65.
The CDC also revised its list of underlying medical conditions that increase risk of severe illness to include:
- Chronic kidney disease
- COPD (chronic obstructive pulmonary disease)
- Obesity (BMI of 30 or higher)
- Immunocompromised state (weakened immune system) from solid organ transplant
- Serious heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies
- Sickle cell disease
- Type 2 diabetes
Additionally, the CDC updated its list of other conditions that might increase a person’s risk of severe illness, adding asthma, high blood pressure, neurologic conditions such as dementia, cerebrovascular disease such as stroke, and pregnancy. A new Morbidity and Mortality Weekly Report found that pregnant women were more likely to be hospitalized, admitted to the intensive care unit, and receive mechanical ventilation than nonpregnant women. At the same time, pregnant women were NOT found to be at greater risk of death from COVID-19.
• American Medical Association (AMA) President Susan R. Bailey, M.D., released a statement on June 25 responding to news reports about health officials being threatened for creating local policies to help stop the spread of COVID-19.
“The AMA is concerned by recent news reports that public health officials have been intimidated and threatened for their work establishing local and state policies intended to stop the spread of COVID-19 and save lives,” Bailey said in the statement. “Particularly during this pandemic, it is important that decision-making be driven by science, data and evidence. Physicians, scientists and public health experts are equipped to interpret this data to help inform steps communities can take to improve health, safety and the well-being of our friends, neighbors and loved ones. … The AMA also calls for an environment in which physicians, scientists and other experts are free to communicate evidence-based, factual information without fear of retaliation or retribution. In words and in actions—and especially at this moment—we should be encouraging careers in public health, not discouraging them.” — Maggie Galehouse
UPDATE | June 25, 2020, 7 p.m.: With headlines about hospital capacity dominating Texas health news this week and a pause on further reopening statewide by Gov. Greg Abbott, let’s take a closer look at regional and Texas Medical Center data.
First, information from the Houston-based SouthEast Texas Regional Advisory Council known as SETRAC, a nonprofit which oversees trauma system networking for the metropolitan area. Its COVID-19 tracker for 25 counties shows an increase in suspected and confirmed coronavirus hospitalizations—now with a specific uptick in the use of general beds.
Over the last month (since May 28), the region’s COVID-19 patient census for general beds nearly quadrupled from 486 to 1,779 while the use of ICU beds nearly doubled from 320 to 637.
An analysis that separates suspected and confirmed cases:
Now, let’s look at the Texas Medical Center’s daily dashboard available at tmc.edu—the Texas Medical Center’s corporate website—which provides pandemic metrics for TMC institutions operating across nine Houston-area counties. Those TMC affiliates are CHI St. Luke’s, Harris Health System, Houston Methodist, MD Anderson Cancer Center, Memorial Hermann, Texas Children’s Hospital and The University of Texas Medical Branch at Galveston (UTMB). Facilities operated under other brands are not included in the data.
While TMC-associated hospitals are ready with testing capability and personal protective equipment (PPE), there are red-light warnings for the daily growth trend in cases, positive tests as a percentage of total tests (14 percent and, this week, exceeding 10 percent for the first time), COVID-19 patients comprising 28 percent of ICU capacity—nearly twice the state’s 15 percent threshold—and the conclusion that, at this rate, ICU capacity could be exceeded in two weeks. — Cindy George
UPDATE | June 24, 2020, 4:25 p.m.: Yesterday, Texas reported 5,489 new cases of COVID-19—another grim record as numbers climb steadily throughout the state. Harris County Public Health is currently reporting 15,419 known active cases in Harris County and Houston combined. During an afternoon news briefing, Mayor Sylvester Turner said the city is reporting 987 new cases and 7 additional deaths today.
“Each one of these persons has a family, relatives, friends,” Turner said, reiterating that these are not just “numbers” being reported, but lives lost.
Testing sites throughout the city are reaching capacity each day, the mayor added, and Houston has asked FEMA to continue providing resources for testing past the current end date on June 30.
“The goal is to—again—to flatten this curve and to slow the progression and to make sure that we don’t become the epicenter of this virus in this country.”
In response to the rising numbers, deemed “unacceptable” by Gov. Greg Abbott during a press conference Monday, he issued an order yesterday giving local officials the authority to regulate public gatherings larger than 100 individuals, a reduction from 500. The governor’s office also is working with the Texas Department of State Health Services to create stricter safety standards for child care centers during the pandemic.
To quell fears about intensive care unit (ICU) availability, the Texas Hospital Association (THA) released a statement reporting that hospitals throughout the state are prepared for an influx of COVID-19 patients and can offer “substantial” capacity in the case of a surge.
“Hospitals are committed to managing capacity so patients get the right care at the right time for COVID-19 and non-COVID-19 medical care. This will help ensure adequate space, staffing and supplies are available for COVID-19 patients,” THA President and CEO Ted Shaw said in the statement. “Through these actions, Texas hospitals have been and will continue to nimbly manage increasing patient volumes as they occur in certain areas of the state. Hospitals are anchors in Texas communities and always are ready to respond to the unique needs of the people they serve.”
The statement noted that hospitals are able to adjust the flow of their patients, including pausing procedures not related to COVID-19 as necessary, which would also increase bed capacity. Texas hospitals also continue to reserve 15 percent capacity for COVID-19 patients.
Still, hospital leaders are urging the general public to remain vigilant, practice social distancing and wear masks in public.
Marc Boom, M.D., president and CEO of Houston Methodist Hospital, appeared on Good Morning America this morning to discuss the alarming numbers in Houston and Harris County with a national audience. Boom said that Houston is not yet at a tipping point and that hospitals in the Texas Medical Center are able to care for patients coming in, but that there is concern about the upward trend in cases.
“I think what’s happened is, and we’re watching it around our community, people have completely let their guard down,” Boom said in the interview.
This afternoon, Texas Medical Center CEOs made a joint appeal for people to maintain social distancing and safe practices while reassuring Houstonians that the TMC is ready to address a surge in cases for now.
A new study suggests widespread under-diagnoses through March
A new study published Monday in the journal Science Translational Medicine, suggests that more than 8.7 million Americans may have had COVID-19 in March, with as many as 80 percent of those cases going undiagnosed. The researchers drew their conclusions based on data collected by the Centers for Disease Control and Prevention (CDC) about patients presenting with influenza-like illness (ILI). The authors wrote that, “As the seasonal surge of endemic non-influenza respiratory pathogens declined toward the later weeks in March, this excess ILI correlated more strongly with state-level patterns of newly confirmed COVID-19 cases, suggesting that this surge is a reflection of ILI due to SARS-CoV-2.”
A survey for Houstonians and a new recovery website
Mayor Sylvester Turner is asking all Houstonians to complete an anonymous, 10-minute survey by Saturday, June 27 to help the city better understand how the pandemic has impacted individual lives. The survey is being conducted by the Mayor’s Health Equity Response (H.E.R.) Initiative and Task Force, which focuses on COVID-19 response and recovery for vulnerable and at-risk populations. The survey is available in English, Spanish, Vietnamese, Chinese (Mandarin) and Arabic.
The City of Houston has also launched a new COVID-19 recovery initiative website to better communicate the city’s comprehensive efforts to respond to the pandemic. The site highlights the city’s multi-pronged initiatives as well as health statistics, testing information, contact tracing efforts, frequently asked questions and related news. —Alexandra Becker
UPDATE | June 23, 2020, 2:34 p.m.: As hospitals grapple with the troubling rise in coronavirus cases in Houston and Harris County, Texas Children’s Hospital is now admitting adult patients to help alleviate the load at other hospitals across the city.
“Yes, Texas Children’s is admitting adult patients,” the statement read. “Texas Children’s Hospital, our employees, medical staff and leadership team continue to carefully monitor the ongoing active transmission and increasing number of COVID-19 cases in the greater Houston area and across the State. We are committed to doing our part to assist the city as the number of COVID-19 cases continues to rise.”
Texas Children’s will be providing additional capacity through ICU and acute care beds to take care of pediatric and adult patients across its hospitals, including an inpatient location in The Woodlands and a West Campus near Katy.
“I’m proud of our @TexasChildrens, stepping up to respond to the challenge of the rise of #COVID19 in #Texas and #Houston: We knew this day would come, I thought perhaps later this summer or fall, but the exponential rise came a bit early,” Peter Hotez, M.D., Ph.D., dean of the National School of Tropical Medicine at Baylor College of Medicine and director of Center for Vaccine Development at Texas Children’s, said in a tweet this morning.
On Monday, the Houston Health Department reported 1,789 new cases of COVID-19, bringing the total number of active cases to 14,313. In addition, the Texas Medical Center’s dashboard showed a 9.1 percent average growth in COVID-19 daily hospitalizations.
According to Texas Health and Human Services on Monday, the number of lab-confirmed COVID-19 patients currently in Texas hospitals reached 3,711—more than double since last month.
“We know COVID-19 has not gone away,” Texas Children’s statement continued. “We implore you to take responsible actions—practice appropriate social distancing, wear a mask or face covering anytime you leave your home, wash your hands frequently for at least 20 seconds, and avoid touching your face.”
AMA calls for change to eliminate COVID-19 health inequities among communities of color
Patrice A. Harris, M.D., immediate past president of the American Medical Association (AMA), testified before the House Budget Committee today during the hearing entitled “Health and Wealth Inequality in America: How COVID-19 Makes Clear the Need for Change” to discuss how COVID-19 has disproportionately affected communities of color.
“Black Americans have been among the hardest hit by this virus,” Harris said during her testimony. “Not only are we hospitalized and dying in disproportionate numbers, we also are more likely than white Americans to have lost income because of the pandemic.”
Harris delineated three key factors driving the health disparities: structural inequities resulting from long-term policies and procedures that determine access to health care and social determinants of health (such as housing, education and food insecurity); higher prevalence of pre-existing health conditions (such as diabetes, hypertension and obesity); and a higher likelihood of working essential jobs (such as transportation workers, custodians and grocers) that increase risk of exposure.
“The AMA is very concerned that the pandemic and the economic fallout will further exacerbate these longstanding and long-term health, economic and social inequities experienced by minoritized and marginalized communities,” she added. “The good news is we are talking about it. … We must use this opportunity to move our country forward on health equity through change at the individual level, in our policies, procedures and in our culture.”
She proposed several ideas to move the needle on health equity, including addressing implicit and unconscious bias at all levels, increasing targeted outreach on COVID-19 testing, ensuring a diverse population of people in vaccine trials, developing a national strategy for a mental health infrastructure and expanding access to high-quality health care.
“We cannot go back to business as usual,” Harris said. “We must work together to build a society that supports equitable opportunities for optimal health for all.” —Shanley Pierce
UPDATE | June 22, 2020, 4 p.m.: Harris County’s new mask order went into effect today, which means that all employees, customers and visitors of commercial businesses will be required to wear a face covering when on the premises. The order, signed by Harris County Judge Lina Hidalgo on Friday, will be effective through June 30 and includes all municipalities and unincorporated areas including Houston.
Businesses that do not comply with the mask requirement could face up to a $1,000 fine; individuals are not subject to fines. Noting that the fines are last resorts, Hidalgo said the order aims to emphasize the importance of face coverings to business owners. The mask order does not apply to children younger than 10.
“Every business has a ‘no shirt, no shoes, no service’ policy—the idea is to see this as ‘no shirt, no shoes, no mask, no service,’” the county judge said during a Friday news conference.
The order also responds to Texas Gov. Greg Abbott’s declaration that counties and cities could not impose penalties on those who refuse to wear masks and should instead focus the responsibility on businesses. Abbott’s office has said orders like this—also implemented in other counties in Texas—are not inconsistent with the state’s mandate and acknowledged the importance of masks in curbing the virus’ spread.
In a news conference this afternoon, he addressed the state’s drastic increase in COVID-19 cases and encouraged Texans to wear masks in public.
“I know that some people feel that wearing a mask is inconvenient or that it’s an infringement of freedom,” the governor said, “but I also know that wearing a mask will help us to keep Texas open.”
Much like the PPE (personal protective equipment) that health care workers on the front lines wear throughout their shifts to protect themselves, their patients and the larger community, face masks for the general public are a critically essential tool proven to interrupt the transmission of COVID-19. According to public health officials, the simple act of wearing a mask will substantially slow the spread of the virus and save countless lives. The Centers for Disease Control and Prevention (CDC) notes multiple studies that have shown a significant number of infections arising from individuals who are either asymptomatic or pre-symptomatic and that those individuals can transmit the virus through speaking, coughing or sneezing. The CDC recommends wearing cloth face coverings in public settings in order to avoid this kind of transmission. Health officials have said that in order for face coverings to be effective, they should fit snugly against the side of the face, be secured with ties or ear loops, and include multiple layers of fabric or a filter while allowing for breathing.
The Harris County face mask order does offer exceptions, including when dining at a restaurant, pumping gas, operating outdoor equipment or being inside a building that requires security surveillance such as a bank. Face coverings also are not required for individuals who are exercising outdoors.
The order is not without controversy, however, as many Texans maintain that any kind of mandate related to the pandemic is an overreach of government power and an infringement on individual liberties, as Abbott acknowledged. Still, the number of COVID-19 infections in Texas, including Houston, has been rising steadily. Over the weekend, Texas reported its largest daily increase in coronavirus cases since the pandemic began, and on Saturday, the Houston Health Department reported 844 new cases as well as 10 additional deaths.
During an afternoon press conference Monday, Houston Mayor Sylvester Turner said these rising numbers are unprecedented for this pandemic.
“Today, we have another grim reminder that the virus is very much alive in our community and that our numbers are moving in the wrong direction,” Turner said. “The Houston Health Department reports 1,789 new cases of COVID-19 today, bringing Houston’s total to 14,322.”
He noted that Monday’s total does include Sunday, but that since Friday, the number of new cases has averaged more than 850 a day. Turner also said the death toll for the city has risen to 196 as of this afternoon.
“During March and April and May, I never reported these types of numbers—never,” Turner said. “We are moving, very fast, in the wrong direction.”
During his news conference today, Abbott acknowledged that while Texas had succeeded in “flattening the curve” through April and May, current data is alarming. He reported that in the last half of May, Texas averaged about 1,500 positive cases a day, but in the past five days in June, the state averaged more than 3,500 cases a day. He added that the positivity rate had increased from approximately 4.5 percent in late May to nearly 9 percent today, and that hospitalizations for COVID-19 averaged just over 1,600 a day in the latter part of May and are now averaging more than 3,200 a day.
“To state the obvious, COVID-19 is now spreading at an unacceptable rate in Texas, and it must be corralled,” Abbott said.
Houston Mayor Sylvester Turner has been an outspoken supporter of face coverings throughout the pandemic, promoting his “MASK UP!” campaign and reinforcing its importance during each public appearance. Over the weekend, he worked alongside volunteers and the city’s Health Equity Response (H.E.R.) Task Force—which focuses on COVID-19 action for vulnerable and at-risk populations—to distribute thousands of face coverings as well as canned goods provided by the Houston Food Bank.
At his afternoon press conference today, Turner reiterated the importance of masks, especially as the number of COVID-19 positive cases continue the climb sharply.
“Let me strongly, strongly encourage you to mask up,” he said. “Because wearing a mask can help slow transmission of the virus, it protects other people from you, it can help save lives, and quite frankly, it’s a sign of respect for other people as well.”
He urged Houstonians to not become lax, thinking the virus is no longer a threat.
“Positive cases are increasing in our city exponentially,” he said. — Alexandra Becker
UPDATE | June 19, 2020, 1 p.m.: Mayor Sylvester Turner joined the mayors of eight other cities across the state in a public letter urging Texans to remain vigilant during the COVID-19 pandemic and to continue to protect themselves and their loved ones.
“We are not asking you to stay home, but we are asking you to mask up and social distance where possible,” the group of mayors wrote to the residents of their respective cities, which include Laredo, Arlington, Grand Prairie, Austin, San Antonio, Sugar Land, Lubbock and El Paso, as well as Houston. “The virus doesn’t leave just because our collective urgency has gone away. … Our failure to do these things will cost all of us. For 40 million Americans, it has cost their job, and for almost 120,000 it has cost their lives. For the rest of us, it has cost us our sense of normalcy in a way we have not felt before.”
—On June 18, the Houston Health Department reported 210 new positive COVID-19 cases, bringing Houston’s total to 10,717. The number of deaths from COVID-19 increased by six, for a total of 175.
—National Cancer Institute (NCI) director Ned Sharpless is concerned that delays in cancer treatments and diagnosis due to the coronavirus pandemic will cause a spike in cancer-related deaths, according to a STAT News story. Delays are of particular concern in cancers for which there is no screening, such as lunch cancer, said Sharpless, who urged hospitals to ramp up cancer care while taking precautions against COVID-19.
—A New England Journal of Medicine article published online on June 18 addresses the challenges of returning to work during a pandemic and offers some solutions gleaned from a group of medical, business, and legal experts. “A strategy of staggering work shifts and allowing both very early and very late shifts reduces workplace density and allows employees and others to use mass transit at off-peak, less crowded hours, thus also reducing commuting risk,” the article states. “Some employers have separated their workforce into teams, with assigned workplace and work-from-home days for each team.” — Maggie Galehouse
UPDATE | June 18, 2020, 4:30 p.m.: Today’s U.S. Supreme Court ruling on DACA, Deferred Action for Childhood Arrivals, impacts dozens of physicians serving on the front lines of COVID-19 in the United States.
In a 5-4 ruling, the court blocked the Trump Administration’s plan to immediately end the Obama-era program that shields about 700,000 immigrants brought to the United States as children from deportation. The court did not “address the merits of the program or the decision to end it,” The New York Times reported, but “ruled only on whether the administration had acted lawfully in trying. The White House is free to try again.”
For now, DACA recipients—mostly young adults known as Dreamers—will continue in a temporary status that allows them to work legally in the U.S. without an immediate threat of being sent back to countries of origin many do not remember. The program does not provide a path for citizenship.
The ruling offers a temporary reprieve to an estimated 200 medical students and residents “amidst a pandemic and physician shortages,” the Association for American Medical Colleges (AAMC) reported. “The Trump administration moved to rescind DACA in 2017 — a decision that the U.S. Supreme Court vacated on June 18, ruling that the Department of Homeland Security did not follow the legally required process. An amicus brief filed by the AAMC on behalf of dozens of health professional education groups supported claims that the federal government terminated DACA without adequately considering the negative consequences of rescinding a long-standing policy. The brief noted that ending the program would leave a hole in the U.S. health care workforce that would be difficult to fill and would disadvantage medical schools and teaching hospitals that have invested in DACA recipients who are training at U.S. institutions.”
Houston has had a delay in reporting some COVID-19 deaths. On Wednesday, Mayor Sylvester Turner announced that the city added seven new cases to its tally. One of the deaths occurred two months ago, April 18, and two six weeks ago on May 1 and May 2, as well as others on May 13, May 29, June 3 and June 15.
Turner also addressed the continuing uptick in Houston-area hospitalizations as well as the increases in cases and testing.
“There have been a number of mass gatherings that have taken place over the last six weeks,” said Turner, who had his second COVID-19 test this weekend, which was negative. “Let me encourage you to be tested … especially if you’ve been a part of the marches, the demonstrations or you’ve been in the bars, clubs or just been in close proximity with a lot of other people.” — Cindy George
UPDATE | June 17, 2020, 4 p.m.: During a press conference Tuesday afternoon, Texas Gov. Greg Abbott addressed the record high number of new COVID-19 cases in the state.
In Texas, there were 2,622 new positive cases and 192 new hospitalizations for a total of 2,518 hospitalizations—the highest number in the state since the start of the COVID-19 pandemic.
Cases in Harris County increased 2.5 percent with 425 new cases. Currently, there are 17,707 total cases and 289 total deaths.
However, the surge of new COVID-19 cases hasn’t deterred Abbott from continuing with his plan to reopen the state—citing “abundant” hospital capacity as a reason to move forward. The number of COVID-19 hospitalizations, he added, is “really a very small percentage of all the beds that are available.”
Abbott attributed the spike in cases to more test results from an assisted living facility in Collin County and an increase in positive cases from Jefferson County, where there are multiple state prisons and a federal prison. On average, the prisons in Beaumont, the seat of Jefferson County, averages 12 to 15 positive cases per day; however, on June 10, 537 tested positive and approximately 520 were inmates.
Abbott also noted that gatherings played a role in the new cases.
“One of the reasons that we have learned from multiple reports across the state of Texas is that there are certain counties where a majority of the people who are tested positive in that county are under the age of 30 and this typically results from people going to bar-type settings,” Abbott said. “It’s hard to tell exactly where those people contracted COVID. It could be Memorial Day celebration. It could be a bar setting. It could be some other type of gathering.”
“We are seeing some increase in the number of COVID patients in the state. We expected this,” added John Hellerstedt, M.D., commissioner of the Texas Department of State Health Services. “But we are seeing it occurring at a manageable level. I really want to stress that the continued success is up to the people of the state of Texas.”
On Tuesday, nine Texas mayors, including Houston Mayor Sylvester Turner, signed a letter urging Abbott to allow them “authority to set rules and regulations” requiring face masks to prevent community spread of the coronavirus.
Although Abbott has previously banned local governments from issuing fines or penalizing people for not wearing face coverings, Harris County Judge Lina Hidalgo is expected enact a mandatory rule after the governor allowed another Texas county to issue an order requiring face masks.
Bexar County is now requiring employees and customers of local businesses to wear face masks “where six feet of separation is not feasible” or risk a fine of up to $1,000.
“Local governments can require stores and business to require masks. That’s what was authorized in my plan,” Abbott said during a KWTX interview Wednesday. “Businesses … they’ve always had the opportunity and the ability—just like they can require people to wear shoes and shirts—these businesses can require people to wear face masks if they come into their businesses. Now local officials are just now realizing that that was authorized.” — Shanley Pierce
UPDATE | June 16, 2020, 4:30 p.m.: A common steroid has been found to provide a statistically significant increase in the survival of COVID-19 patients who are seriously ill, according to a new study from the United Kingdom.
“A cheap, readily available steroid drug reduced deaths by a third in patients hospitalized with Covid-19 in a large study, the first time a therapy has been shown to possibly improve the odds of survival with the condition in the sickest patients,” a STAT News story reported. “The drug, dexamethasone, is widely available and is used to treat conditions including rheumatoid arthritis, asthma, and some cancers.”
Some, though, criticized the swift rush to hail the findings, noting that the study’s full data have not been published or exposed to scientific review. Oxford University issued a news release about the clinical trial.
Atul Gawande, M.D., MPH, a surgeon, writer and public health researcher, urged caution in a tweet, STAT News reported. “After all the retractions and walk backs, it is unacceptable to tout study results by press release without releasing the paper,” Gawande wrote.
The news comes one day after the U.S. Food and Drug Administration (FDA) withdrew its emergency approval for two malaria drugs, hydroxychloroquine sulfate (HCQ) and chloroquine phosphate (CQ), for COVID-19 treatment.
If you get a call from a health department, answer the phone. Also respond if you receive a text or email. That’s the plea from the Houston Health Department as contact tracers work hard to do the excruciatingly detailed person-to-person work that helps track the spread of COVID-19.
Contact tracing is not new. It’s a routine public health practice that’s essential for stopping the spread of infectious diseases like the novel coronavirus that causes COVID-19 illness. Contact tracers work with people who have COVID-19 to let their close contacts know they may have been exposed.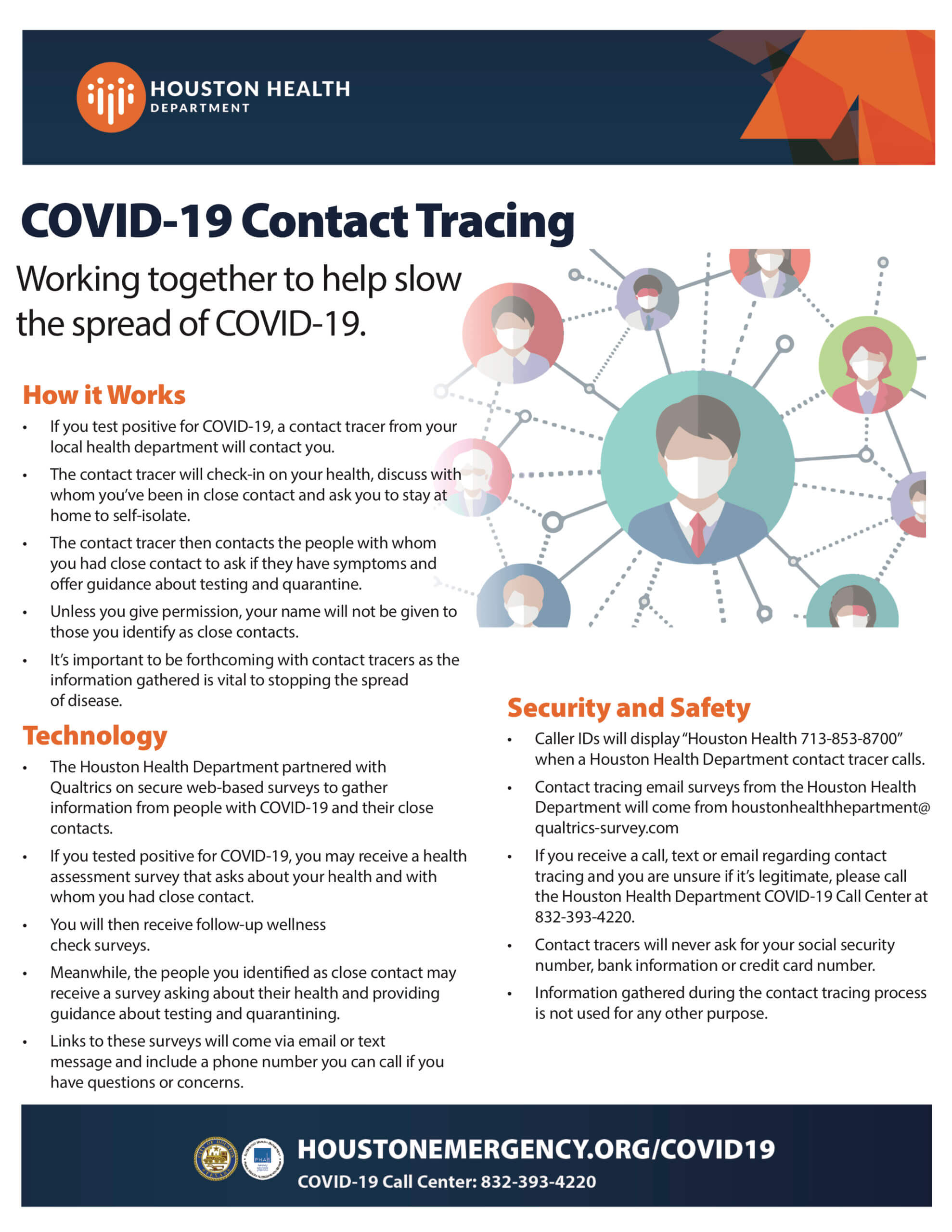
-
-
- Caller IDs will display “Houston Health 713-853-8700” when a Houston Health Department contact tracer calls.
- Contact tracing email surveys from this email address — houstonhealthhepartment@qualtrics-survey.com — are from the Houston Health Department.
- If you receive a call, text or email regarding contact tracing and you are unsure if it’s legitimate, please call the Houston Health Department COVID-19 Call Center at 832-393-4220.
- Contact tracers will never ask for your Social Security number, bank information or credit card number.
- Information gathered during the contact tracing process is not used for any other purpose.
-
For more information, visit houstonemergency.org/covid19 or call the city’s COVID-19 Call Center at 832-393-4220. — Cindy George
UPDATE | June 15, 2020, Noon: The U.S. Food and Drug Administration (FDA) said today that it has withdrawn the emergency approval for use of the drugs hydroxychloroquine sulfate (HCQ) and chloroquine phosphate (CQ) as treatment for COVID-19. Both hydroxychloroquine and chloroquine are clinically prescribed to treat malaria. The FDA said that the drugs are unlikely to be an effective treatment for COVID-19 and noted their severe side effects, among them serious cardiac adverse events.
The Centers for Disease Control and Prevention (CDC) also released new guidelines to help the general public understand levels of risk for going out in public, reiterating that while communities may be reopening, the pandemic is far from over.
The recommendations emphasize that “the more closely you interact with others and the longer that interaction, the higher the risk of COVID-19 spread.” They encourage individuals to think about how many people they are interacting with, if they can keep six feet of space between other people and how long they’ll be around others. The CDC strongly encourages everyone to wear face coverings when out in public, as they have been proven to greatly reduce transmission of the virus. The guidelines also outlined specific recommendations for common errands and activities, including going to the bank, dining out at a restaurant, hosting a gathering or cookout, using a gym, going to the nail salon, visiting libraries and overnight travel.
Mayor Sylvester Turner held a morning press briefing today to announce details on this year’s Shell Freedom Over Texas event on the Fourth of July.
“This year’s event will be different than in years past, but I can promise you that it will be a quality, entertaining production,” Turner said. “Due to the current COVID-19 pandemic, events throughout the city and the entire nation have been forced to postpone, cancel and reorganize, and these are unprecedented times for us all. But in times such as these we find that our spirit of community is even stronger. And with all that we have been through since March 1, I believe that it is especially important that we move forward in our celebration of America’s birthday.”
To adhere to CDC guidelines and follow social distancing recommendations, the event on July 4 will not include an outdoor festival or live audience, but will be broadcast by ABC Channel 13 and also streamed online. The show will feature a performance at Jones Hall by the Houston Symphony with special guest entertainers and collaborators. In addition, there will be a 15-minute professionally produced fireworks finale sponsored by Reliant Energy, which can be viewed digitally or live from porches, balconies, backyards, parking lots or in cars. Individuals who wish to view the fireworks outside are encouraged to “mask up” and practice social distancing while doing so.
“It is a unique year. It’s unique with COVID-19, but it does not change the fact that we should be celebrating our independence and the sacrifice that so many have made and the sacrifice that many are still making,” Turner said. “So even though we are making the variations, the spirit of this Independence Day, the reason why we are doing it, those things have not changed. We as Americans, we find a way to continue to celebrate while being healthy at the same time.” — Alexandra Becker
UPDATE | June 12, 2020, 12:15 p.m.: Mandated face coverings in three COVID-19 epicenters—Wuhan, China and Italy and New York City—reduced the number of COVID-19 patients in those areas, according to a new study published in the Proceedings of the National Academy of Sciences of the United States of America. The study determined that masks reduced the number of infections by 78,000 in Italy between April 6 and May 10 and by more than 66,000 in New York City between April 17 and May 9.
Free COVID-19 supplies
Houston Mayor Sylvester Turner, along with other elected officials and volunteers, will distribute free masks, hand sanitizer and educational materials from 11 a.m. to 1 p.m., Saturday, June 13, at Missouri City Baptist Church, 16816 Quail Park Drive, in Missouri City. The event, presented by the city’s Health Equity Response (H.E.R.) Task Force – Medical Care Subcommittee and the Houston Medical Forum, aims to provide relief to individuals facing increased food insecurity and limited ability to acquire items for novel coronavirus protection and to maintain general health.
Slow Streets project
With so many Houstonians social distancing and working from home, many more people than usual are walking and biking. To accommodate this shift in pedestrian and transportation flow, Houston is launching a Slow Streets pilot project that limits certain streets to local traffic in order to provide more space for walkers and cyclists. The project will last until Labor Day.

The Slow Streets project aims to accommodate the increase in foot and bike traffic in certain Houston neighborhoods. (Courtesy photo)
The first streets in the pilot project are located in the Eastwood neighborhood of Houston and include McKinney (Milby to Dumble) and Dumble (Polk to Harrisburg). At certain intersections on these streets, the city has placed movable barriers that retain space for local traffic and encourage through traffic to take alternate routes.
For more information on the Slow Streets pilot project, click here. — Maggie Galehouse
UPDATE | June 11, 2020, 4:30 p.m.: Harris County Judge Lina Hidalgo unveiled a new simple-to-read, color-coded system to help residents understand the COVID-19 threat to the community.
The Harris County COVID-19 Threat Level System is a four-color, green-yellow-orange-red dial of right-to-left increasing urgency. Today’s Level 2, orange, is in the “significant” range, which means residents should minimize all contacts.
The new system comes from concerns about escalating positive cases and an increasing number of general and intensive care unit (ICU) beds in local hospitals occupied by COVID-19 patients.
“I am growing increasingly concerned that we may be approaching the precipice of a disaster,” Hidalgo said.
The Houston-Harris County region has done well compared to other major U.S. cities, but the hospital population started climbing in the last two weeks. There’s particular pressure in the public health safety net Harris Health System’s hospitals, Ben Taub and LBJ.
“This week, the COVID-19 general hospital population in Harris County was the highest it has ever been. It was the highest on Monday and it’s gotten worse every day,” Hidalgo said.
That description coincides with a state milestone reached Tuesday, the first day of the number of people hospitalized with COVID-19 in Texas exceeded 2,000. That mostly was fueled by admissions in Houston and Dallas, according to the Texas Department of State Health Services, the Dallas Mornings News reported.

Harris County COVID-19 Threat Level on June 11, 2020
Hidalgo, who leads the nation’s third most-populated county, was joined at Thursday’s news conference by Houston Mayor Sylvester Turner; David Persse, M.D., the city’s public health authority; Umair Shah, M.D., MPH, executive director of Harris County Public Health; and Stephen Williams, the director of the Houston Health Department.
The county judge noted that there is plenty of ICU and hospital capacity right now, but that may not last if a continually increasing number of people continue to get sick.
“If the trends we’re seeing right now get worse or continue to rise, we are at a very high risk of getting to the point where the threat to our hospital system is severe and we have to backtrack. We hope that trend will stop … but we’ve only had more and more—reopening Phase 2, then Memorial Day and then even more contact,” Hidalgo said. “So perhaps it’s unlikely to expect things to change unless we all change our behavior and take personal responsibility to keep our county and our metrics from continuing to head in a dangerous direction.”
Turner urged people to start or continue the well-worn prevention protocols: Wear a mask, sanitize your hands, employ social distancing.
“It is more important now than even before,” he said. “Otherwise, we’ll get to the position where the spread will exceed our hospital capabilities and we will find ourselves in deep trouble.”
Persse, who is also board chair of the SouthEast Texas Regional Advisory Council known as SETRAC, noted that the people being admitted to hospitals for COVID-19 are in general beds “moreso than the ICU beds” and that they’re younger. The data shows that the average age of patients admitted to the hospital is dropping.
“That is, again, consistent with the reopening of society and folks going out and behaving in ways, that really, we wouldn’t recommend: Again, large groups, not wearing masks, not social distancing,” Persse said, adding that he attributes the improvement in numbers for older residents to the testing and prevention efforts in nursing homes.
Visit ReadyHarris.org for a more detailed explanation of the Harris County COVID-19 Threat Level System and the indicators involved in setting the gauge.
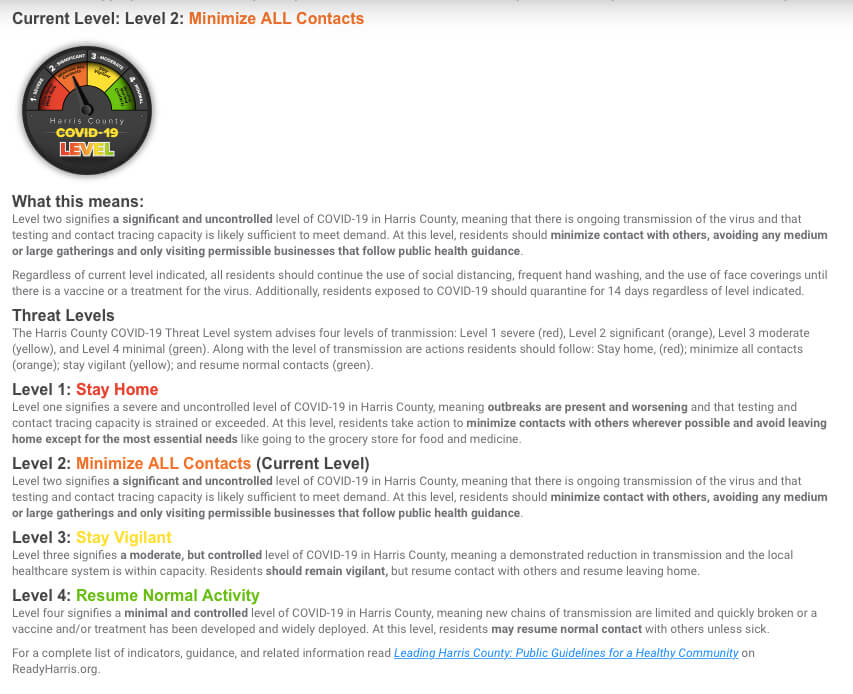
Harris County COVID-19 Threat Level System indicators
“We may be tired of this virus, but this virus is not tired of us,” Shah said. “This gauge allows for an easier-to-understand way for our community to know where we are in the coming weeks and months of this pandemic and what kind of activities are going to allow for protection.” — Cindy George
UPDATE | June 10, 2020, 3:30 p.m.: Harris County Judge Lina Hidalgo’s “Stay Home, Work Safe” order expires today at 11:59 p.m., but a new order is expected to be announced this week.
According to the Texas Medical Center dashboard, there has been a 4.5 percent increase in daily new COVID-19 hospitalizations. Data from the Texas Department of State Health Services showed that Monday and Tuesday had the highest number of cases—614 and 622, respectively—since the state initiated Phase 1 of reopening. In addition, the state exceeded 2,000 hospitalizations on Tuesday for the first time.
Experts warned early on that an uptick would occur as soon as the state began lifting restrictions. The recent protests and demonstrations in response to George Floyd’s death by police officers left some public health officials worried that a surge in new COVID-19 cases could occur.
Houston Mayor Sylvester Turner said that these protests are not a factor in the increase of new cases.
“Covid-19 positive cases have been increasing for the last 2 weeks as well as hospitalizations. This current rise cannot and should not be attributable to the mass protest and demonstrators,” Turner wrote in a tweet.
Mixed messaging
The World Health Organization (WHO) is now backpedaling from a position that asymptomatic spread of COVID-19 appears to be “very rare” after the statement on Monday left many, especially experts, scratching their heads.
Maria Van Kerkhove, the technical lead for WHO’s COVID-19 response team, made the initial remarks. She clarified her controversial statement Tuesday during a social media Q&A.
“The majority of transmission that we know about is that people who have symptoms transmit the virus to other people through infectious droplets, but there are a subset of people who don’t develop symptoms and to truly understand how many people don’t have symptoms, we don’t actually have that answered yet,” Van Kerkhove said.
The initial statement contradicted messaging and guidelines from public health and government officials who strongly encouraged social distancing and wearing face coverings to prevent unintentionally spreading the virus to others. Policies designed to flatten the curve were based on asymptomatic transmission playing a major role in the community spread. A recent study determined that asymptomatic spread of COVID-19 accounts for at least 30 percent of cases but is more likely to be in the range of 40 to 45 percent. — Shanley Pierce
UPDATE | June 9, 2020, 11:20 a.m.: The World Health Organization (WHO) said Monday during a press conference that asymptomatic spread of COVID-19 disease is “rare,” despite earlier messaging from experts that infected individuals who do not show symptoms have been a large driver of the pandemic. The statement, based on extensive contact tracing, acknowledged, however, that asymptomatic individuals infected with COVID-19 can and do transmit the virus to others.
Maria Van Kerkhove, head of the emerging diseases and the zoonoses unit at the WHO, stated: “We have a number of reports from countries who are doing very detailed contact tracing. They’re following asymptomatic cases. They’re following contacts. And they’re not finding secondary transmission onward. It’s very rare.”
The position has proven controversial since multiple studies have shown asymptomatic transmission is not uncommon, including one published recently in the Annals of Internal Medicine.
On Monday, two studies were released showing that government restrictions likely have saved millions of lives around the world. A report published in the journal Nature found that approximately 62 million infections in the U.S. were prevented as a result of social distancing and city lockdowns. Another study, also published in Nature, argued that shutdowns had a large effect on drastically reducing disease transmission in Europe.
The U.S. Department of Veterans Affairs has announced that military funeral honors can resume today after deferment due to COVID-19 restrictions and precautions. Led by members of the Department of Defense, military honors generally include the folding and presentation of a U.S. burial flag to family members and a performance of Taps. Cemeteries will still be asked to follow CDC guidelines, including social distancing, limiting attendees and wearing face coverings. — Alexandra Becker
UPDATE | June 8, 2020, 1:48 p.m.: Last Wednesday, Gov. Greg Abbott announced Phase 3 of his plan to reopen Texas. Effective immediately, nearly all businesses will now be allowed to operate at 50 percent capacity.
Restaurants, which had been given the green light to increase capacity to 50 percent during Phase 2, will be able to expand table size from six people to 10. Starting June 12, they will be able to move up to 75 percent capacity.
Bars will be allowed to increase capacity to 50 percent as long as “patrons are seated.”
The capacity limit only pertains to indoor bar and restaurant seating; outdoor patios and backyards do not have capacity limits.
In addition, amusement parks and carnivals in counties with fewer than 1,000 confirmed positive cases may expand their capacity to 50 percent. Starting June 19, these types of establishments in counties with more than 1,000 confirmed positive cases will be given the green light to open at 50 percent capacity, as well.
More testing sites
As the state reopens more of its economy, containing the spread of COVID-19 remains an ever-present challenge. Testing continues to play a crucial role in ensuring that people are returning to businesses safely.
The Houston Health Department (HHD) and agency partners are expanding the number of COVID-19 testing sites starting June 8.
Testing is free and available to anyone regardless of whether or not they exhibit symptoms.
From June 8 to June 13, the Texas Division of Emergency Management (TDEM) will open four drive-through test sites from 9 a.m. to 6 p.m. at the following locations:
-
-
- Spring Oaks Middle School (2150 Shadowdale Dr.)
- HCC-Northeast Campus (555 Community College Dr.)
- Codwell Elementary School (5225 Tavenor Ln.)
- Kingwood Park Community Center (4102 Rustic Woods Dr.)
-
Appointments are required and can be made online at txcovidtest.org or by phone at 512-883-2400.
Weekday testing will be available through United Memorial Medical Center (UMMC) at the following locations:
-
-
- Southwest Multi-Service Center (6400 High Star) from 10 a.m. to 5 p.m.
- Houston Community College-Southeast (6815 Rustic) from 9 a.m. to 4 p.m.
- UMMC Tidwell (510 W Tidwell Rd.) from 9 a.m. to 4 p.m.
- Forest Brook Middle School (7525 Tidwell Rd.) from 10 a.m. to 5 p.m.
- Cullen Middle School (6900 Scott St.) from 10 a.m. from 5 p.m.
- Griggs School (801 Regional Park Dr.) 10 a.m. from 5 p.m.
-
UMMC sites do not require appointments and have the capacity to test 250 tests daily.
Houston Health Department offers drive-through testing at two community-based sites, each with a capacity to test 500 tests per day, from Monday to Saturday.
To receive an access code and directions to the closest site, call 832-393-4220 between 7 a.m. and 4 p.m.
Four local Federally Qualified Health Centers (FQHC) testing sites have received additional test kits, lab access and equipment in order to offer more tests. To schedule an appointment, call:
-
-
- Spring Branch Community Health Center (713-462-6565)
- El Centro de Corazon (713-660-1880)
- Avenue 360 Health and Wellness (713-426-0027)
- Lone Star Circle of Care at the University of Houston (346-348-1200)
- Community Health Network (281-816-3317)
-
Patients will not be turned away due to inability to pay or lack of insurance.
Visit HoustonEmergency.org/covid19 for more information on testing site locations and schedules. – Shanley Pierce
UPDATE | June 5, 2020, 3:45 p.m.: This evening, Houston Mayor Sylvester Turner will help high school seniors in the area celebrate their 2020 graduations at a handful of outdoor events held by the following school districts: Aldine, Alief, HISD, Spring Branch and Spring.
Each live event will feature a video tribute to the graduates with messages from celebrities including Houston Rockets’ James Harden, rappers Trae tha Truth and 50 Cent, actress Chandra Wilson, Houston Texans’ JJ Watt and others.
“With the support of district superintendents, their teams, and some pretty big-name celebrities, I know this will be a memorable event that the senior class of 2020 can experience together, and thanks to our media partners, the entire Houston community can share virtually as well,” Mayor Turner said in a press release.
Turner initiated this event to recognize high school seniors in the area who have missed many traditional memories due to the COVID-19 pandemic.
For updated information on COVID-19 cases in the area: Click here for the Texas Department of State Health Services real-time COVID-19 dashboard and here for combined Harris County/Houston data.
New guidance
On June 4, the U.S. Department of Health and Human Services (HHS) offered new guidance that outlines COVID-19 data that laboratories across the country are compelled to report to HHS to ensure public health officials have real-time information at their fingertips.
New reporting requirements incorporate demographic data including race, ethnicity, age and sex. Not only will this help determine which groups are most burdened and vulnerable to infection, but it will help HHS officials better monitor disease incidence and trends. — Maggie Galehouse
UPDATE | June 4, 2020, 6:30 p.m.: There’s been a new increase in COVID-19 hospitalizations and cases credited to the reopening of businesses and Memorial Day weekend gatherings, according to new data.
A tweet just before 6 p.m. from Harris County Judge Lina Hidalgo from her handle @LinaHidalgoTX said:
“Over the past 7 days we’ve seen a statistically significant (95% confidence level) increase in COVID-19 hospital admissions. I remain very concerned about the impact of reopening too quickly. Please take personal responsibility. Social distance. Wear face coverings. Avoid groups.”
The TMC daily dashboard available at tmc.edu, the Texas Medical Center’s corporate website, provides updated data on the availability of ICU beds, ventilators, personal protective equipment and other pandemic metrics for TMC institutions operating across nine Houston-area counties. Those TMC affiliates are CHI St. Luke’s, Harris Health System, Houston Methodist, MD Anderson Cancer Center, Memorial Hermann, Texas Children’s Hospital and The University of Texas Medical Branch at Galveston (UTMB). Facilities operated under other brands are not included in the data.
The Texas Medical Center’s daily dashboard on Thursday said that the upswing in the “current COVID-19 caseload growth trajectory suggests base ICU capacity could be exceeded in 2 weeks.”
State guidelines require 15 percent of intensive care unit (ICU) capacity to be reserved for COVID-19 patients. TMC-affiliated institutions have reached that threshold.
The Houston-based SouthEast Texas Regional Advisory Council known as SETRAC, a nonprofit which oversees trauma system networking for the metropolitan area, also has a COVID-19 tracker for 25 counties that shows an increase in hospitalizations and an uptick in the use of ICU beds.
Other warning signs include an increase in the percentage of positive COVID-19 tests on both platforms. — Cindy George
UPDATE | June 3, 2020, 2:00 p.m.: Yesterday at 4 p.m., individuals from Texas Medical Center institutions, including McGovern Medical School at UTHealth, Baylor College of Medicine and The University of Texas Medical Branch at Galveston (UTMB), gathered at the Hermann Park Reflection Pool for a peaceful demonstration against systemic racial injustice to highlight how racism drives health disparities and in support of the Black Lives Matter movement. At the gathering—called White Coats for Black Lives—participants stood in silence for 8 minutes and 46 seconds, the length of time a white police officer kneeled on George Floyd’s neck causing his death in Minneapolis last week.
Anthony Fauci, M.D., director of the National Institute of Allergy and Infectious Diseases (NIAID) and a member of the White House Coronavirus Task Force, said yesterday that the United States should have at least 100 million doses of a COVID-19 vaccine candidate by the end of this year. By the beginning of 2021, he said he hopes that will increase to a couple hundred million doses. This first vaccine candidate will be made by the biotech company Moderna.
As of today, there have been 13,027 confirmed cases of COVID-19 and 236 deaths in Houston and Harris County combined. The latest numbers can be found on Harris County Public Health’s website.
Facebook rolled out new maps and tools today to help researchers explore movement patterns in communities. The mobility data, aggregated from users who access the Facebook app from their phones, is helping researchers map the spread of COVID-19.
The Centers for Disease Control and Prevention (CDC) also released a report today on the impact COVID-19 has had on emergency department visits in the United States.
The National Syndromic Surveillance Program, which collects electronic health data in real time, found that emergency department visits declined 42 percent during the early weeks of the COVID-19 pandemic. While diagnoses associated with lower respiratory disease, difficulty breathing and pneumonia increased, the number of visits for conditions like nonspecific chest pain and acute myocardial infarction (heart attack) decreased, suggesting that individuals could be delaying care for conditions that could be life-threatening if left untreated. The report noted that people who use emergency services as a safety net because of lack of access to primary care may be disproportionately affected if they are avoiding care due to COVID-19 exposure concerns. The authors recommended that while health care settings should continue to adhere to infection control practices recommended by the CDC, messaging should reinforce the importance of seeking emergent care for critical conditions, including any symptoms related to heart attacks. — Alexandra Becker
UPDATE | June 1, 2020, 4:50 p.m.: As people across the country leave quarantine to protest police brutality during unrest ignited by last week’s death of George Floyd in Minneapolis, Houston officials and public health experts are concerned that the crowded demonstrations could increase the number of COVID-19 cases.
Over the past weekend, protestors gathered in more than a dozen cities nationwide—including Houston—to voice their outrage. As cities brace for continued protests, demonstrators are encouraged to wear face coverings and practice social distancing to protect themselves and others from the virus-carrying respiratory droplets that are emitted through people’s mouths.
“As people return to work this week and participate in demonstrations in memory of George Floyd, it is more important than ever to wear your face coverings, maintain social distancing and practice good hygiene,” Houston Mayor Sylvester Turner said during his daily press briefing. “We do not want a surge of COVID-19 in our community because we dropped our guard and failed to adhere to the health warnings.”
People should also continue to get tested, he added.
“With all of the enhanced activity that is taking place right here in the city of Houston,” Turner said, “let me encourage you—if you’ve been around crowds, mass gatherings, especially where people may not have had a mask or you did not engage in social distancing—to take full advantage of one of those 27 free testing sites located throughout the city.”
Hurricane season preparation
With June 1 marking the first day of hurricane season, Turner and the City of Houston Office of Emergency Management (OEM) also urged residents to prepare for the severe storms predicted amidst the global coronavirus pandemic.
OEM has been tracking Tropical Depression Amanda, which has already caused destructive flooding in El Salvador and Guatemala with a rising death toll this past weekend. It’s the first named tropical storm of the 2020 East Pacific hurricane season.
“Models show that it will possibly come into the Gulf,” said George Buenik, director of the Mayor’s Office of Public Safety and Homeland Security. “We’re looking at Friday and Saturday. We’re going to be tracking it each and every day as we get closer to the weekend. We’ll have a better idea of where the storm is going to go. There’s a dozen different models out there and a little less than half of them show it going into the Gulf.”
OEM issued a set of guidelines to help people prepare for hurricane season while protecting themselves and others from COVID-19, including:
-
-
- Plan ahead to dedicate more time than usual to collect emergency food, water and medical supplies. While home delivery is the safest option, remember to wear face coverings, practice good hygiene and social distance when shopping in stores.
- Prepare a “go kit” with essential emergency items, as usual, but include extra hand sanitizer, hand soap and two cloth face coverings per person to protect yourself and others from COVID-19. Children under 2 years old should not use face coverings.
- Practice social distancing and wear face coverings when checking on neighbors and friends.
-
The Centers for Disease Control and Prevention (CDC) also offers preparation and safety tips for protecting yourself and others while in a public shelter.
National Day of Mourning
As the country is gripped by outrage over the death of George Floyd in the middle of a global health crisis, municipality and faith leaders across the country declared today a National Day of Mourning and Lament to remember the people who died due to COVID-19. The death toll in the country has now exceeded 100,000, according to the CDC.
“Today, I join with other mayors across the nation in declaring this a National Day of Mourning for those who have lost their lives to COVID-19,” Turner said. “We encourage faith and community leaders and all Houstonians to pause, reflect, pray, mourn and honor all those who have died and to comfort those family members who have been left behind.” — Shanley Pierce
UPDATE | May 29, 2020, 12:30 p.m.: Many Americans consider going to the hospital to be risky behavior during the era of COVID-19. A new survey by the Society for Cardiovascular Angiography & Intervention (SCAI) found that 36 percent of respondents believed going to the hospital was dangerous—more dangerous than visiting a salon.
Close to 1,000 adults over the age of 30 were polled in the survey, which speaks to a growing concern among hospitals and physicians that some patients in need of care for medical emergencies—including heart attacks and strokes—are too afraid to go to the hospital for fear of contracting COVID-19.
Other highlights from the survey include:
-
-
- 61 percent of respondents believe they’re somewhat likely or very likely to acquire COVID-19 in a hospital
- Half of respondents are more afraid of contracting COVID-19 than having a heart attack or stroke
- Almost 60 percent of respondents are more afraid of a loved contracting COVID-19 than experiencing a heart attack or stroke
-
Trump terminates U.S. relationship with WHO
President Trump announced today that the United States would stop funding the World Health Organization and cut ties with the agency, which he criticized for not doing enough to halt the coronavirus pandemic. In response, Patrice A. Harris, M.D., M.A., president of the American Medical Association, issued the following statement:
“In the grip of a global pandemic that has already killed more than 100,000 Americans, severing ties with the World Health Organization (WHO) serves no logical purpose and makes finding a way out of this public health crisis dramatically more challenging. This senseless action will have significant, harmful repercussions now and far beyond this perilous moment, particularly as the WHO is leading worldwide vaccine development and drug trials to combat the pandemic. COVID-19 affects us all and does not respect borders; defeating it requires the entire world working together. In the strongest terms possible, the American Medical Association urges the President to reverse course and not abandon our country’s leadership position in the global fight against COVID-19.”
Make art matter on June 20
As part of The National Arts Drive, Houston will join other cities in encouraging artists and arts organizations to perform, display or showcase their creativity from driveways, lawns, stoops or other safe locations during one three-hour period: Saturday, June 20, from 3 to 6 p.m.
Those who appreciate art are encouraged to support the artists and groups by driving around their communities and stopping to enjoy the art or performance from a safe distance. The driving experience is paired with a mobile website and interactive map where drivers can also engage with the artist/organization and support them by liking, following, and sharing their work via social media; donating directly to the artist or organization through their chosen mobile paysite; or visiting the online store or website of a participating artist or organization for a future purchase.
This nationwide project was launched by RAWartists.com in response to an Americans for the Arts COVID-19 impact survey, which found that 62 percent of artists in the United States are now unemployed.
Artists and organizations that want to participate can sign up at www.nationalartsdrive.com/signup-artist, and list Houston Mayor’s Office of Cultural Affairs as your ambassador. Community drivers can RSVP at nationalartsdrive.com.
In-person spectators allowed in outdoor sports venues
Starting May 31, Texas counties will be allowed to host spectators at professional sporting events in outdoor venues, so long as the venues reach no more than 25 percent capacity. Before this can happen, though, the Texas Department of State Health Services (DSHS) must grant approval to each professional league. A “Checklist for Professional Sports Leagues” on the DSHS website states:
“Each professional sports league that desires to reopen must first submit a plan to the Texas Department of State Health Services (“DSHS”). Spectators are allowed for outdoor events, provided that outdoor venues limit the number of spectators to no more than 25% of the normal operating limits of the venue as determined by the facility owner. Spectators are not permitted for indoor events. Each plan must incorporate these minimum health protocols to the greatest extent possible.” — Maggie Galehouse
UPDATE | May 28, 2020, 6:30 p.m.: Harris County’s improved COVID-19 dashboard now has a tool that allows the exploration of confirmed cases by ZIP Code as well as by race and ethnicity.
Following the expansion of city testing sites this week, Harris County announced that its two largest test locations will move from Baytown and Katy to Pasadena and the Cypress-Fairbanks area (Cy-Fair) beginning June 1.
To receive free testing, appointments are required. Residents should register and use the self-assessment tool available at readyharris.org or by calling 832-927-7575. (Those wishing to get tested the following day should call or register online after 6:30 p.m.)
During the screening process, residents can select a date and time to get tested. Residents must have an authorization code to get tested and walk-ups will be turned away. Residents from other counties can also be tested at any of these sites.
The two new sites opening next month will be able to conduct 750 tests per day each, up from 500 each in Baytown and Katy, at the following locations:
Cy-Fair
Pridgeon Stadium
11355 Falcon Rd A, Houston, TX 77065
Pasadena
San Jacinto College Central
8060 Spencer Hwy, Pasadena, TX 77505
To date, Harris County has offered testing at 29 locations across the county.
“Testing is a key component of Harris County’s COVID-19 containment strategy, which includes contact tracing and treatment,” a county news release said. “Testing enables health officials to identify new cases of COVID-19 so contact tracers can determine the sources of infection and help prevent further spread of the virus.”
Harris County operates a total of six testing sites throughout the county with the capacity to test up to 1,700 residents each day. Harris County Public Health encourages any residents who believe they have COVID-19 or have been exposed to someone with the virus to get tested.
Click here for the Texas Department of State Health Services real-time COVID dashboard and here for combined Harris County/Houston data. — Cindy George
UPDATE | May 27, 2020, 4 p.m.: Texas Department of State Health Services is distributing an additional 75 cases of the antiviral drug, remdesivir, to 27 Greater Houston Area hospitals to help treat patients with COVID-19.
“The Lone Star State continues to prioritize the health of our fellow Texans and ensure that medical providers across the state have the supplies needed to respond to COVID-19,” Gov. Greg Abbott said in a statement. “I am grateful to our partners at the U.S. Department of Health and Human Services for providing these cases of remdesivir to communities across the state of Texas. Texas will continue to act swiftly to provide for our hospitals, secure treatment for patients, and slow the spread of COVID-19.”
Touted as the most promising weapon against COVID-19 and the new “standard of care” for COVID-19 by the nation’s top infectious disease specialist Anthony Fauci, M.D., remdesivir received emergency use authorization by the U.S. Food and Drug Administration on May 1, two days after the results of the National Institutes of Health’s clinical trial gave researchers hope for the drug, which had been previously studied to treat the SARS, MERS and Ebola viruses.
A recent study published in the New England Journal of Medicine tested the drug on 1,059 patients in a randomized trial, with 538 assigned to remdesivir and 521 who received a placebo. The results of the study showed that the drug shortened the recovery time to 11 days instead of 15 days.
Although state health departments decide the number of cases each county receives based on COVID-19 hospitalizations, DSHS had previously allocated only 57 cases for hospitals in the Greater Houston Area, forcing doctors to ration an insufficient supply of the potentially lifesaving experimental drug.
Counties receiving a portion of the additional 75 cases of remdesivir are:
-
-
-
-
-
-
-
-
- Brazoria County: 2
- Fort Bend County: 3
- Galveston County: 14
- Harris County: 50
- Matagorda County: 1
- Montgomery County: 3
- Walker County: 2
-
-
-
-
-
-
-
Once hospitals receive the cases of remdesivir, it’s up to the doctors and medical staff to decide which patients will receive the drug. Adult and pediatric patients who are hospitalized with severe cases of COVID-19 are top priority for receiving the drug, in accordance with FDA guidelines. —Shanley Pierce
UPDATE | May 26, 2020, 11 a.m.: The Health Museum will be hosting an emergency blood drive today through Thursday, May 28. Held in partnership with the Gulf Coast Regional Blood Center, the blood drive is intended to alleviate local shortages created by the COVID-19 crisis. Those interested in donating must sign up in advance to make an appointment. Participants will receive a free guest pass for two to visit The Health Museum.
WHERE: The Health Museum, 1515 Hermann Drive, Houston, Texas 77004.
WHEN: By appointment only from 10 a.m. to 2:30 p.m., today through Thursday
SIGN UP: https://www.giveblood.org/the-health-museum/
In addition, the Houston Health Department, together with agency partners, is setting up new sites for free COVID-19 testing throughout Houston this week.
In partnership with the Texas Division of Emergency Management, two drive-thru sites will be open at the following locations:
-
-
-
-
-
-
-
-
- Kingwood Park Community Center, 4102 Rustic Woods Drive, Kingwood, May 26-27
- Sagemont Church Annex, 11600 Hughes Road, May 28-30
-
-
-
-
-
-
-
Testing is by appointment only and from 9 a.m. to 6 p.m., or until each site reaches its daily capacity of 250 tests. To register, call 512-883-2400 or visit txcovidtest.org.
United Memorial Medical Center (UMMC) will open a new drive-thru and walk-up test site at the Denver Harbor Multi-Service Center, located at 6402 Market Street, and will continue to offer drive-thru testing at Houston Community College-Southeast, located at 6815 Rustic. Each site will be open from 9 a.m. to 4 p.m. or until capacity is reached. More information can be found by calling 1-866-333-COVID or visiting ummcscreening.com.
Kroger Health will host a free drive-thru test site at the Collier Regional Library, 6200 Pinemont Drive, from 10 a.m. to 5 p.m. daily. Appointments are required and can be made at krogerhealth.com/covidtesting.
The Houston Health Department will continue to operate two free drive-thru COVID-19 community-based testing sites open to anyone, regardless of symptoms. Call the department’s COVID-19 Call Center at 832-393-4220 between 7 a.m. to 4 p.m. to receive an access code and directions to the nearest site.
The health department is also working with four local Federally Qualified Health Centers (FQHC) to help them expand their testing capacity. Appointments can be made at the following locations:
-
-
-
-
-
-
-
-
- Spring Branch Community Health Center: 713-462-6565
- El Centro de Corazon: 713-660-1880
- Avenue 360 Health and Wellness: 713-426-0027 and
- Lone Star Circle of Care at the University of Houston: 346-348-1200.
-
-
-
-
-
-
-
Visit HoustonEmergency.org/covid19 for the most up-to-date information about COVID-19 test sites. — Alexandra Becker
UPDATE | May 22, 2020, 3:30 p.m.: Led by Texas researchers, an international team of scientists, chemists, biochemists and virologists have joined forces to help find a cure for COVID-19 by identifying drug-like molecules that inhibit SARS-CoV-2 replication.
The COVID-19 Drug Discovery Consortium is harnessing powerful supercomputers to screen millions of small molecules against all the major non-structural proteins of SARS-CoV-2 in hopes of finding molecules that stop the virus.
Using Texas Advanced Computing Center (TACC) supercomputers, the consortium has already identified the 600 molecules most likely to disrupt the virus. The next step involves testing these molecules against the virus in high containment facilities. The most potent antiviral compounds will then move to manufacturing and safety/toxicity studies in preparation for first-in-human clinical studies.
The consortium grew out of a group of researchers who had previously used the Drug Discovery @ TACC portal. The seven founders include Stan Watowich, Ph.D., and Mark White, Ph.D., of The University of Texas Medical Branch at Galveston; and Xiaodong Cheng, Ph.D., of The University of Texas MD Anderson Cancer Center.
Death of Keith Wade
Keith Wade was a special advisor to Mayor Sylvester Turner and Mayor Annise Parker.
Keith Wade, a special advisor to Houston Mayor Sylvester Turner, has died of COVID-19, city officials announced Thursday.
“Keith and I go back 46 years, to our days on the campus of the University of Houston,” Turner said, in a statement. “After I was speaker of the student government, he was president. Our journey in politics started on the UH campus.”
In addition to championing the causes of labor and the disenfranchised, Wade advocated for voting rights, Turner said.
“He was instrumental in so many campaigns in all levels of government—and that is true in my case, as well,” Turner said. “He was actively involved in my 2015 campaign and when I ran for re-election in 2019.”
Wade was a special advisor to both Turner and Mayor Annise Parker, who served from 2010 to 2016.
“This is a sad day for a lot of people because Keith wasn’t just a consultant or a special advisor, he was a friend and a brother,” Turner said.
Billy Kelly, director of government relations for Turner, tweeted: “So much of Houston was made better because of Keith Wade.”
Distinguished Leadership Award
William F. McKeon, president and CEO of the Texas Medical Center, received a Distinguished Leadership Award from Baylor College of Medicine during the May 21 virtual commencement for the Baylor College of Medicine class of 2020. McKeon won for his outstanding work responding to the coronavirus pandemic.
Paul Klotman, president, CEO and executive dean of Baylor College of Medicine, officiated at the virtual ceremony. Two additional Distinguished Leadership Awards went to Grace Chimene, president of the Texas League of Women Voters, and Esmaeil Porsa, M.D., president and CEO of Harris Health System.
Covid-19 data
Harris County, including Houston, is reporting more than 6,000 active COVID-19 cases and a total of 216 deaths. Click here for the Texas Department of State Health Services real-time COVID dashboard and here for combined Harris County/Houston data. — Maggie Galehouse
UPDATE | May 21, 2020, 4 p.m.: Despite a mask covering her nose and mouth, sad eyes and a quivering voice, Gayle Pierce implored everyone to wear face coverings at Houston Mayor Sylvester Turner’s news conference on Thursday.
“Stop being macho. Stop trying to be cute. Put the mask on,” said the widow of Tony L. Pierce. She was joined on stage by their daughter, Nia Pierce. “The bottom line is: You need to mask up.”
Gayle Pierce describes the loss of her husband, Tony L. Pierce, to COVID-19 during Mayor Sylvester Turner’s news conference on May 21, 2020.
The last time Gayle Pierce spoke to her husband face-to-face was March 28, when she drove him to a local hospital. He was “sedated, intubated and on a ventilator,” she said, and died 25 days later from pneumonia and other complications of COVID-19.
“It makes me mad every time I go to the store and I see dozens and dozens of people walking around unmasked,” she said. “Why can you not wear a mask and protect yourselves and others?”
Tony L. Pierce, 57, was a beloved husband, father, friend, education manager at Houston Firefighters’ Relief & Retirement Fund, Houston Livestock Show and Rodeo committee volunteer and a brother of Alpha Phi Alpha Fraternity, Inc. Also a black man, he is part of a racial demographic disproportionately represented in the tally of COVID-19 hospitalizations and fatalities.
As we enter the Memorial Day holiday weekend, city pools and splash pads will remain closed. Effective June 1, all three city-owned golf courses and the trio of large tennis complexes will open for play with restrictions.
Turner’s message remains the same: Continue to physically distance, wash your hands and wear face coverings in public—a directive amplified by the city’s #MaskUp campaign.
According to a new analysis of cellphone data, Houston is one of several cities in the South that may see a spike in cases in June.
“If people in Houston and Palm Beach, Fla., for example, aren’t being cautious with masking in indoor crowded locations and with hygiene and disinfection, local governments may need to intervene again should they lose control of the epidemic,” said a blog post by PolicyLab at the Children’s Hospital of Philadelphia.
In response to the gradual reopening of Texas, Harris County Judge Lina Hidalgo on Thursday released suggested worker protection guidelines to “serve as a bridge from policy to practice … for a baseline expectation of safety” for public-facing businesses such as retail and restaurants, along with a second set for those in construction and manufacturing.
“It’s not enough to call essential workers our heroes. We have to create an environment in which they’re safe—and they don’t feel like they have to choose between safety and putting food on the table,” the county judge said. She was flanked by representatives of unions and building trades as well as electrical and iron workers. “These guidelines are designed to help lift the real dangers and the sheer fear that workers are exposed to and suffer from day to day when they try to keep our economy going and they try to keep us safe.”
The county guidelines include screening workers for symptoms and conducting routine disinfection as well as scheduling flexible shifts and staggering work times when practical. Minimum protocols include no adverse action against employees who have been quarantined for possible COVID-19 exposure, screening for symptoms, workers wearing face coverings and employees not returning to work if they are sick.
Read the entire guidelines for retail businesses here and for construction companies here.
The National Oceanic and Atmospheric Administration (NOAA) announced an expected “above-normal” hurricane season, with a 60 percent chance of more activity than usual. The Atlantic hurricane season begins on June 1 and lasts through November 30.
Additionally, an emergency blood drive will be held next week from Tuesday, May 26 to Thursday, May 28 to address an urgent need created by COVID-19. Gulf Coast Regional Blood Center seeks donors to make appointments from 10 a.m. to 2:30 p.m. at The Health Museum, 1515 Hermann Drive in Houston. The center needs 800 to 1,000 daily donations to be able to provide blood and blood products to 170 hospitals and health care institutions in the region. In appreciation, all donors will receive a free pass for two to visit The Health Museum.
Harris County, including Houston, has crossed two grim thresholds: More than 10,000 cases and deaths exceeding 200. Click here for the Texas Department of State Health Services real-time COVID dashboard and here for combined Harris County/Houston data. — Cindy George
UPDATE | May 20, 2020, 4:45 p.m.: As Phase 2 of Gov. Greg Abbott’s plan continues to ease restrictions on businesses, including increasing restaurant occupancy limits from 25 percent to 50 percent and allowing entertainment-based businesses to reopen on May 22, many people are eager for the return to normalcy. However, Houston Mayor Sylvester Turner urged Houstonians to not let their guard down and to continue practicing safety measures that were put in place before Abbott’s tiered plan to reopen the state.
“We have noticed toward the end of March and April that people were wearing face coverings, engaging in social distancing and staying at home,” Turner said during his press conference this afternoon. “Now, what we’re seeing is that it’s on and off—people are not wearing masks as much, which is unfortunate. That’s why we’re putting forth an extra push to encourage people to mask up—to put on masks and face coverings because the very same things we needed to do in March and April to flatten the [curve] are the same things we need to continue to do in order to keep everyone safe.”
The next phase of Abbott’s push to restart the state’s economy includes opening summer camps, youth programs and Little League programs on May 31. In addition, professional sports—such as golf, baseball, tennis, football and basketball—will be able to resume without in-person spectators. Health experts, including city health authority David Persse, M.D., have warned that there will be an uptick of new COVID-19 cases as more businesses reopen.
In keeping with his push to increase testing, Turner announced that the city plans to have 24 testing sites by the end of the month.
The mayor also announced that Walgreens is opening an additional drive-through testing site at 8301 Broadway St. on the southeast corner of Broadway and Bellfort. People 18 and older may make appointments online through the Walgreens website whether or not they are exhibiting symptoms and can receive their test results within 15 minutes.
In the city of Houston, there are 146 new cases and two new deaths, totaling 6,047 cases and 119 deaths. —Shanley Pierce
UPDATE | May 19, 2020, 2:15 p.m.: Lives lost during this pandemic cannot be celebrated as usual, which is why we pause today to honor one of the Texas Medical Center’s pioneering leaders. Cheves McCord Smythe, M.D., the founding dean of The University of Texas Health Science Center at Houston‘s medical school, died in Charleston, South Carolina, on May 11. He was 95.
A graduate of Harvard Medical School, Smythe served at the Naval Medical Center Camp Lejeune during the Korean War. He also trained at Bellevue Hospital in New York City and at Boston City Hospital, where he was named chief resident.
In 1970, he moved from South Carolina to Texas to lead The University of Texas Medical School at Houston, now McGovern Medical School, as its inaugural dean.

Cheves Smythe, M.D. (Courtesy photo)
During two separate leaves of absence from the school, between 1982 and 1985 and between 1990 and 1991, Smythe also served as founding dean and chair of the department of medicine at the Aga Khan University of Health Sciences in Karachi, Pakistan.
Smythe worked at McGovern Medical School for more than four decades, returning as a professor of internal medicine and a dean pro-tem later in his career before retiring in 2012. He also served as chief of medical services at Lyndon B. Johnson Hospital and was certified in geriatric medicine and internal medicine. In 2006, the Cheves Smythe Distinguished Lecture was established to attract distinguished speakers with topics focused on aging.
Smythe is survived by his wife, Isabella (Polly) Carr Smythe and their five sons, 14 grandchildren and three great-grandchildren.
In other news today, the Harris County Commission approved a $30 million COVID-19 relief fund, which will provide up to $1,500 to families in Harris County most in need, including those who make 60 percent below the area median income, youth who have recently aged out of foster care, survivors of domestic violence and individuals living in homeless shelters.
Additionally, centenarian Annie Glenn, the widow of the late astronaut John Glenn—the first American to orbit the Earth—died of COVID-19 complications. The 100-year-old was a lifetime advocate for individuals with disabilities. —Alexandra Becker
UPDATE | May 18, 2020, 7 p.m.: Phase 2 of the state’s reopening plan for businesses begins this week. Daycares and massage centers can open immediately. Restaurant occupancy restrictions now increase from 25 percent to 50 percent. Bars, bowling alleys, skating rinks and other entertainment venues can reopen partially by the end of the week.
Houston Mayor Sylvester Turner responded to the governor’s executive order by recommending face masks and coverings, social distancing and continued caution.
“I want to see the economy move forward and I want people to get back to work so that they can provide for their families, but I also want to make sure that it is done in a safe and responsible way. Since March, Houston has taken steps and made sacrifices to prevent the spread of COVID-19,” the mayor said. “Our efforts have saved lives and prevented our local health care system from being overwhelmed. I don’t want us to lose sight of the fact that the virus is still in our community and I think we all recognize that. … We must continue to remain vigilant even as restrictions are being lifted.”
The City of Houston and its partners have more than a dozen testing sites open this week at various locations.
Harris County Judge Lina Hidalgo also responded to state action concerning the Texas Supreme Court’s removal of emergency protections halting evictions and debt collection proceedings during the COVID-19 pandemic. Hidalgo announced on March 19 that all 16 justices of the peace—the courts where evictions are filed—had halted those proceedings through March 31. A subsequent statewide ban on evictions is set to expire today. Last week, the Texas Supreme Court ruled that evictions could resume on May 19. (That ruling excludes residents who receive federal rent assistance.) The order also give justices of the peace discretion about how to proceed locally.
“Restarting eviction and debt-collection proceedings right now will only deepen the well of desperation many families are experiencing across our county,” Hidalgo said in a statement. “These are hard-working families who, through no fault of their own, have lost irreplaceable income during this pandemic and may not qualify for federal assistance or eviction protections. Thousands of Harris County residents are already on the ropes, and becoming homeless will crush their chances for short-term recovery and long-term economic independence. Evicting families is also a threat to public health – we’re working day and night to stop the spread of this virus and, at a time when we’re asking residents to stay or work from home to limit spread, we cannot afford to contribute to a surge in homelessness.”
More than 89,000 people have died from a documented COVID-19 illness in the United States, including more than 1,300 deaths in Texas, 90 deceased in Harris County and 115 deaths in Houston. That follows more than 1.4 million reported infections nationwide, including nearly 49,000 cases in Texas, 3,840 cases in Harris County and 5,795 cases in Houston. Click here for the Texas Department of State Health Services real-time COVID dashboard and here for combined Harris County/Houston data. — Cindy George
UPDATE | May 15, 2020, 2:00 p.m.: To date, there have been 8,817 cases of COVID-19 and 193 deaths in Harris County and the city of Houston combined.
On Thursday, the Centers for Disease Control and Prevention (CDC) issued a health advisory to clinical providers warning of a multisystem inflammatory syndrome in children (MIS-C) likely connected to COVID-19. The condition was first believed to be Kawasaki disease or toxic-shock syndrome. The CDC is asking that all health care providers who have treated or are caring for patients 21 and younger suspected of having MIS-C report those cases to their local health department.
The CDC’s case definition for MIS-C includes:
-
-
-
-
-
-
-
-
- A patient less than 21 years old presenting with fever, laboratory evidence of inflammation and evidence of clinically severe illness requiring hospitalization with more than two organs involved (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic or neurological)
- No alternative plausible diagnosis
- A positive test for current or recent SARS-CoV-2 infection or exposure to COVID-19 within the past four weeks
-
-
-
-
-
-
-
It is currently unknown if this multisystem inflammatory syndrome can also occur in adults.
Four to five potential vaccines for COVID-19 look promising, according to the director of the National Institutes of Health (NIH), and at least one will be ready for large-scale testing by July, with others to follow.
Governor Greg Abbott has confirmed that nonessential manufacturing plants, office buildings and gyms in Texas can reopen on Monday, May 18 at 25 percent capacity. All must adhere to social distancing guidelines set forth by the governor’s reopening plan. For gyms, locker rooms and showers will remain closed and patrons will be required to wear gloves that completely cover hands while using the equipment. — Alexandra Becker
UPDATE | May 14, 2020, 4:15 p.m.: Nearly 85,000 people have died from a documented COVID-19 illness in the United States, including more than 1,200 deaths in Texas, 84 deceased in Harris County and 109 deaths in Houston. That follows 1.4 million reported infections nationwide, including more than 43,000 cases in Texas, 3,640 cases in Harris County and 5,177 cases in Houston. Click here for the Texas Department of State Health Services real-time COVID dashboard and here for combined Harris County/Houston data.
On Thursday, Texas reported a record 58 COVID-19 deaths—the highest statewide number in one day since the pandemic began, the Houston Chronicle reported.
“This is something that continues to be preventable. We have to continue to fight aggressively to protect the lives of our friends and our neighbors—our parents and our grandparents,” Harris County Judge Lina Hidalgo said this week as she greeted the county’s second class of contact tracers. They are part of the area’s army of disease detectives. These workers have been deployed as part of the county’s test-trace-treat initiative “to ensure that reopening wouldn’t necessarily mean a spike in cases that overwhelmed our health care system,” Hidalgo said.
Additional COVID-19 news highlights:
• Of the city’s 109 deaths, 25 are associated with nursing homes and two with the Harris County Jail. The close quarters of congregate care facilities for seniors as well as jails and prisons have been ongoing areas of concern for the spread of the virus.
• Live in Harris County and need a free COVID-19 test? Schedule an appointment through the online screening tool or by calling 832-927-7575 for access to drive-through or mobile testing sites.
• The Houston Health Department shared this NPR report about how to use the right cloth for safer homemade face masks.
• Houston Mayor Sylvester Turner has tested negative for COVID-19, following a report of illness from Houston City Council at-large member Letitia Plummer, DDS. Houston City Council meetings will be virtual for the next two weeks. — Cindy George
UPDATE | May 13, 2020, 4 p.m.: The Houston Health Department announced 117 new cases of COVID-19 and three new deaths, bringing the total to 5,030 cases and 104 deaths. The deceased individuals include two black females in their 70s with underlying health conditions and one white female in her 90s with underlying health conditions. Of the 104 deaths, 24 cases are associated with nursing homes.
The city continues to contain the spread of COVID-19 along with efforts to alleviate the economic burden, namely unemployment, that has a resulted from the pandemic.
“As we work to save lives and stop the spread of COVID-19 in our community, many Houstonians are also coping with the reality of job losses during the public health crisis,” Houston Mayor Sylvester Turner said during his daily press conference this afternoon.
Last week, Houston City Council passed a $15 million rental assistance program using a portion of the $404 million the city received through the CARES Act. Landlords registered last week to accept the relief funds. The program opened for applicants at 10 a.m. today and was exhausted within 90 minutes as more than 17,000 renters flocked to the website to apply for assistance.
“I knew going into it that the need would be greater than the amount provided,” Turner said, adding that he sent a letter urging federal leaders to commit at least another $100 billion to rent relief and $75 billion to homeowners facing foreclosure.
In an effort to simultaneously increase employment opportunities and bolster COVID-19 containment initiatives, the Houston Health Department (HHD) will host two virtual job fairs to hire 300 contact tracers to add to its existing team of 125.
The two Houston Together Virtual Job Fairs will be held at 11 a.m. and 1 p.m. Thursday, May 14 on the City of Houston Human Resources website.
“The whole idea of contact tracers or contact investigation is to ensure that we get an informed history of close contacts of a person who has tested positive, so that we can conduct an intervention that will lead to those individuals being safe,” said HHD Director Stephen Williams.
The 300 new temporary positions are critical to the city’s contact tracing efforts, Williams added, to help support call centers for testing sites and to serve as community involvement coordinators.
“This is not new for the health department,” Williams said. “We’ve been doing this since the early inventions of public health, but it’s never been to this scale or scope.”
Currently, the two major testing sites include Butler and Delmar stadiums, which have tested more than 30,000 individuals.
The city’s mobile testing sites are expected to hit 25 locations by the end of May and each has the capacity to test 100 to 150 people per day.
“The goal is to have testing everywhere,” Turner said. — Shanley Pierce
UPDATE | May 12, 2020, 3 p.m.: The City of Houston is reporting an additional 153 positive cases of COVID-19, bringing the total case count to 4,913. Additionally, one new death is reported for the city—a male in his 30s—bringing that total to 101. Yesterday, an individual between the ages of 10 and 19 died in Houston from COVID-19.
“This is a reminder that this virus doesn’t discriminate in terms of age,” Mayor Sylvester Turner said during a news briefing.
Starting next week, city council meetings will become virtual gatherings.
On Monday, the mayor’s office confirmed that Houston City Council member Letitia Plummer, DDS, tested positive for COVID-19. In a statement, Turner said: “I am praying for Council Member Letitia Plummer’s speedy recovery as she isolates at home. Based on my observations, she has been careful to protect her health and the safety of those around her by practicing social distancing and wearing facial coverings.”
The mayor also said he plans to follow protocol and will be tested for COVID-19 this week.
Turner also announced details for the city’s proposed budget for fiscal year 2021, which is impacted by the coronavirus crisis.
-
-
-
-
-
-
-
-
- The proposed budget for all funds totals $5.1 billion, which is an increase of $62.2 million, or 1.2 percent.
- The COVID-19 pandemic has created a $169 million gap in the budget.
- Turner said the city will be experiencing a cumulative estimated loss in sales tax revenue of approximately $107 million.
- To address the shortfall, there will be a deferment of five police cadet classes and an anticipated 3,000 city employees would be furloughed for up to 10 days beginning in FY 2021. Roles related to the city’s police and fire departments as well as solid waste services will not be impacted by the unpaid days off.
-
-
-
-
-
-
-
“We are presenting a budget that does balance,” Turner said. “Even in a very uncertain time, we are obligated to balance our books—and we are doing that.” — Alexandra Becker
UPDATE | May 11, 2020, noon: Houston is reporting 4,531 confirmed cases of COVID-19 and a total of 94 deaths related to the disease—up four from May 8.
The Houston Health Department (HHD) and agency partners will set up new COVID-19 testing sites in vulnerable local communities this week.
• The Texas Division of Emergency Management and HHD will open a drive-through test site at Moreno Elementary School, 620 E. Canino Rd., for residents in the Northside and Northline areas. The agencies will also set up a site at Holland Middle School, 1600 Gellhorn Dr., for the Pleasantville area. The sites will open today through Saturday, May 16, from 10 a.m. to 7 p.m. or until each reaches its daily capacity of 250 tests. Both sites require appointments; call 512-883-2400 or visit txcovidtest.org.
• United Memorial Medical Center (UMMC) will open a new drive-through and walk-up test site at the Stimley-Blue Ridge Neighborhood Library, 7007 W. Fuqua Street, in Missouri City. This location will be open today through Saturday, May 16, from 10 a.m. to 5 p.m. or until reaching its daily capacity of 250 tests. No appointments or symptoms are required for testing. For additional information about UMMC test sites, call 1-866-333-COVID or visit ummcscreening.com.
• HHD will relocate its mobile unit to the Third Ward Multi-Service Center, 3611 Ennis, from Tuesday, May 12 through Friday, May 15, from 10 a.m. to 4 p.m.; and Saturday, May 16, from 10 a.m. to 2 p.m., or until reaching daily capacity of 100 tests. No appointments or symptoms are required for testing.
• Next week, HHD the mobile unit will be located at the Northeast Multi-Service Center, 9720 Spaulding Street, from Tuesday, May 19, to Friday, May 22, from 10 a.m. to 4 p.m.; and Saturday, May 23, from 10 a.m. to 2 p.m., or until reaching daily capacity of 100 tests. No appointments or symptoms are required for testing. — Maggie Galehouse
UPDATE | May 8, 2020, 5:30 p.m.: Houston is reporting 4,419 confirmed cases of COVID-19 today and a total of 90 deaths related to the disease—up 5 from yesterday.
As of May 7, 2020 in the United States, there have been 1,219,066 confirmed cases of COVID-19 detected through U.S. public health surveillance systems in 50 states and the District of Columbia, Puerto Rico, Guam, the Northern Mariana Islands, and the U.S. Virgin Islands, according to the Centers for Disease Control and Prevention. For more detailed information, click here.
As we move into Mother’s Day weekend, here are a few news stories that tackle the most recent wrinkles of the COVID-19 era:
—Health workers on the front lines in the United States and Europe have been reporting a rare pediatric inflammatory condition that may be linked to COVID-19. Kawasaki disease is characterized by swelling, fever and rash. Read more about Kawasaki disease and its possible connection to COVID-19 in this story from Time.
—Across the U.S., companies have closed worksites for the past several weeks or so, or operated at significantly reduced capacity. As states start to lift stay-at-home orders, companies have to figure out how to keep employees and customers safe. Read more in this report from Kaiser Health News.
—Despite chatter about when the second wave of this pandemic will hit, the U.S. is still in the throes of the first wave. Read more in Stat News. —Maggie Galehouse
UPDATE | May 7, 2020, 4:30 p.m.: At a Thursday afternoon news briefing, Mayor Sylvester Turner announced 88 new cases of COVID-19, bringing the cases for the city of Houston to 4,227. In addition, he reported three more deaths, bringing that total to 85.
“This is just a reminder with these numbers that this virus is still prevalent in our community and we need to continue to engage in social distancing and wearing our face coverings,” Turner said. “That’s critically important.”
Joining the mayor virtually was Tina Knowles Lawson, who spoke about her work with daughter Beyoncé’s BeyGOOD foundation to offer expanded COVID-19 testing in Houston this coming Mother’s Day weekend.
Knowles Lawson stressed the importance of testing in order to curb the spread of COVID-19 within communities.
“If we can play some part in keeping those numbers down, that would make me really, really happy,” she said. “I’m just so proud of Houston for being at the forefront and for keeping the numbers down, but I just encourage everyone to go get tested. It’s really, really important.”
COVID-19 Recovery Czar Marvin Odum also introduced an expanded program aimed at increasing testing access and equity as well as the Houston Health Department’s plan to significantly add to its contact tracing workforce. Turner and Odum said both testing and contact tracing were critical to protecting Houstonians as the city moves into the first phases of reopening.
“COVID-19 remains a real and present danger in all our lives,” Odum said. “As we continue to reopen Houston, we must do it safely and with a plan to protect the health of Houstonians. We must become even more strategic in our efforts to control the spread of the virus.”
Odum said the Houston Health Department is developing a community-based approach to dramatically increase the accessibility of testing across the city. More than 24 new testing sites will be added by the end of May, guided by the principles of access and equity. The new locations will be a mixture of fixed sites, mobile testing units and strategic outreach teams prioritized to address the city’s most vulnerable and at-risk neighborhoods first. Odum said these choices will be determined from data provided by the Centers for Disease Control and Prevention (CDC), UTHealth and the city’s health department.
“These are neighborhoods where people are more likely to die if they get COVID-19, and in many cases until now, have had relatively little access to testing,” Odum said. “We’re changing that.”
He added that these tests will be free and available to anyone.
Odum also addressed the city’s expanded efforts around contact tracing, which involves the monitoring and containment of COVID-19 as more of the economy restarts.
“This is the work of contact tracers, often called public health disease detectives,” Odum said. “This process involves interviewing patients to determine where they’ve been and with whom they’ve been in close contact, so those people can get tested and the spread can be contained.”
Odum announced that the City of Houston will be adding 300 additional contact tracers to its already 125-strong workforce.
“To find these people, we’re going to tap into the talent of our local educational institutions and likely will be conducting job fairs as well,” Odum said.
David Persse, M.D., the city’s health authority, also spoke at the afternoon briefing and stressed the importance of individual behavior in containing future spread of COVID-19.
“At the end of the day, it’s the individual’s responsibility,” Persse said. “No matter how big we make the army, we’re not going to be able to sit in front of your house and make sure you follow the rules.” — Alexandra Becker
UPDATE | May 6, 2020, 4:05 p.m.: Houston Mayor Sylvester Turner announced a historic, first-of-its-kind celebration for the graduating class of 2020.
Due to the COVID-19 pandemic, school districts were forced to cancel activities, field trips, proms and other events to protect the health and safety of students and faculty. However, high school seniors will have the opportunity to return to their respective campuses on Friday, June 5, 2020 for an outdoor celebration.
“No doubt, there has been uncertainty as to how to celebrate the accomplishments of the class of 2020 with COVID-19. This unique class of scholars has persevered through one of the most challenging times in recent history with remarkable resilience,” Turner said during his daily press conference this afternoon. “The students earned their title of graduating seniors, and it is appropriate for the city of Houston to celebrate and honor their achievements in a way that reflects the culmination of this moment and the unity of our city.”
On the evening of June 5, members of every graduating class across the city will simultaneously return to campus grounds in their caps and gowns—while accessorizing with face coverings and practicing social distancing—for “a collective-but-personal celebration that salutes the achievement of graduates and reflects the unity of our city,” Turner explained.
While only graduating seniors and faculty will be allowed to participate in the outdoor celebration, parents, family members and friends will be able to join virtually.
In collaboration with the Mayor’s Office of Special Events and Houston First, the citywide event will also feature congratulatory messages from special guests and remarks from school superintendents.
“Our students may not have the prom to look back on and the field trips they have lost,” Turner said, “but I think, collectively, we can work together to put on a very special moment that says to our students: ‘We believe in you. We want to encourage you. As you go forward, we want you to know that our city stands behind you.’”
Turner was joined by local superintendents to make the special announcement.
“This is going to be a unique opportunity that they can look back on,” said LaTonya Goffney, Ed.D., the Aldine Independent School District’s superintendent. “I can reflect on the fact that my grandmother used to say, ‘Where there is unity, there is strength,’ so in addition to celebrating our class of 2020, I think it’s an opportunity to bring to life the hashtag, #HoustonStrong.”
Turner also provided the latest COVID-19 numbers. According to the Houston Health Department, there were 77 new cases and 3 new deaths, bringing the total to 4,139 cases and 82 deaths. — Shanley Pierce
UPDATE | May 5, 2020, 7 p.m.: Texas barbershops, nail salons, hair salons, cosmetology salons and tanning salons will be allowed to open on Friday, May 8, under restricted circumstances.
Gov. Greg Abbott’s modified executive order for a phased reopening of the state allows those businesses to resume at 25 percent capacity. Businesses should have one customer per stylist; appointment systems are preferred and waiting clients should employ social distancing inside or go outside. Abbott “strongly” recommends stylists and clients wear face masks.
Worship services, funerals and burials as well as weddings remain under some social distancing measures. Restaurants were allowed to open as of May 1 with 25 percent capacity limitations indoors— that guideline doesn’t apply to outdoor seating. All still must comply with social distancing.
Gyms will be allowed to open under restrictions beginning May 18 with showers and locker rooms closed during the initial phase.
Abbott said he was guided by data showing that, as of Tuesday morning, there remained more than 19,000 hospital beds, 2,000 ICU beds and more than 6,600 ventilators available statewide.
“Testing continues to ramp up,” he said. “From March 1 to April 20, there were 190,000 people who were tested for COVID-19. Since that time, there have been well over 220,000 tested.”
Public health professionals note that 400,000 people in two months is less than 2 percent of the state’s 29 million people.
“Texas is fully capable of being able to manage the health care needs of everybody who contracts COVID-19,” the governor said. “There has never been any evidence whatsoever that Texas either has or will be facing the types of challenges that we’ve see in places like New York, New Jersey, New Orleans or some of these other places where they were scrambling to amass the resources that were needed to respond to COVID-19.”
In a news conference shortly after Abbott’s announcement, Houston Mayor Sylvester Turner emphasized continued “social separation” and wearing “face coverings or masks” for city residents.
“The reason why we have been successful in keeping our numbers lower than cities across the country is because of the steps you have been taking,” the mayor said. “I am concerned … with what I saw this weekend on the beaches, for example: Way too many people. … I am concerned as we continue to open more, it seems as though we are doing less. Opening up our city or opening up our state does not mean things are normal and it doesn’t mean that we shouldn’t be continuing to safeguard ourselves …. so we don’t put ourselves in a sense where this virus will resurface three to four weeks down the road.”
George Buenik, director of the Mayor’s Office of Public Safety and Homeland Security—which includes the Office of Emergency Management—noted that this is Hurricane Preparedness Week and urged residents to “make a plan, build a kit, stay informed” as hurricane season begins on June 1.
On Wednesday, the Houston City Council will vote on a $15 million rental assistance program for families with low and moderate incomes at risk of eviction who have lost jobs or faced financial challenges because of COVID-19. The program would provide housing stability for 7,000 to 13,000 families, the mayor said. — Cindy George
UPDATE | May 4, 2020, 5:30 p.m.: The city of Houston is reporting 3,992 cases of COVID-19; fatalities have reached 75.
Across Texas, the current reported number of COVID-19 cases is 32,332, with a total of 884 fatalities. The state estimates that more than 16,000 patients have recovered from COVID-19, while more than 1,500 patients are still suffering from the disease in Texas hospitals.
The Texas Division of Emergency Management and the Houston Health Department are introducing free drive-through testing to the Hobby Airport area and expanding operations at the existing Sunnyside testing site, which opened April 29. A free, mobile test site will commence operation at Ortiz Middle School, 6767 Telephone Road, from May 5 to May 9. The Sunnyside site, at Worthing High School, 9215 Scott Street, will extend its testing through May 9. Individuals must make an appointment if they wish to be tested at either site by visiting txcovidtest.org or calling 512-883-240..

Houston Mayor Sylvester Turner helped distribute food on May 2 at a food drive organized by the Houston Food Bank and the Houston Independent School District. (Courtesy photo: Houston Food Bank)
On Saturday, May 2, Houston Mayor Sylvester Turner made four public appearances at COVID-19 events.
In the morning, he joined Houston City Council member Abbie Kamin to distribute masks at 1101 Taft Street. Later that morning, Turner and Council member Karla Cisneros helped pass out masks and hand sanitizer at 2915 Main Street.
At noon, the mayor took part in a food distribution drive at Community of Faith Church, 1024 Pinemont Drive.
On Saturday afternoon, Turner helped distribute food at NRG Stadium at a food drive organized by the Houston Independent School District and the Houston Food Bank. — Maggie Galehouse
UPDATE | May 1, 2020, 3:15 p.m.: Harris County’s ‘Stay Home, Work Safe’ order officially ended today as Phase 1 of the governor’s reopening plan begins, but local leaders including health care executives urge the community to remain vigilant and to continue the safety practices established over the past two months.
At a Friday morning news conference, Harris County Judge Lina Hidalgo reiterated that the pandemic is not over as Texas reported 50 deaths on Thursday and more than 1,000 new cases of COVID-19. In addition, Harris County reported 97 new cases and 1 additional death outside the city of Houston.
“It’s a grim reminder that this virus doesn’t respect dates on a calendar,” Hidalgo said. “It’s impossible to pull a date out of thin air and say to the virus: ‘We’re ready for you to go away now.’ That’s not how it works. That’s not how any of this works. We can’t allow ourselves to be desensitized to what’s happening, to lose our sense of humanity. Fifty Texans—brothers, sisters, parents, grandparents, sons and daughters—had their lives cut short yesterday from a single, invisible killer that still lurks among us.”
Hidalgo urged people in Harris County to reopen slowly for the sake of public health.
“If the virus spreads like wildfire and the hospitals run out of space, or are running out of space again, things are going to have to shut back down—again,” Hidalgo said. “If we do the re-opening step by step, carefully, there’s a chance of succeeding by slowly reopening if we’re able to contain and we’re able to test and we’re able to trace.”
Hidalgo noted that the Texas attorney general issued a clarifying letter to try to clear confusion about what businesses could open and which should remain closed.
“If you’re not essential, as defined by the order I issued or by the governor’s order, and you are not reopen as classified under the governor’s order—the three reopenings he listed—you should be closed,” the county judge said.
She added that she would reissue her order later today to conform with the governor’s order and the attorney general’s clarification.
“Just because you can open, doesn’t mean you should,” she said, also announcing that she was adding another “T” for “teamwork” to her “test, trace, treat” reopening strategy.
“That ‘T’ involves every single resident in Harris County,” she said. “If these doctors and these nurses get overwhelmed, people die en masse. Plain and simple.”
Joining Hidalgo at this morning’s briefing was Esmaeil Porsa, M.D., MBA, MPH, president and CEO of Harris Health System; Umair A. Shah, M.D., MPH, executive director of Harris County Public Health; Marc L. Boom, M.D., president and CEO of Houston Methodist Hospital; and Paul Klotman, M.D., FACP, president and CEO of Baylor College of Medicine.
“We have managed to flatten the curve and that is great news. I am cautiously optimistic that we may have done well in our efforts to contain the coronavirus, but our work is far from over,” said Porsa, who leads Harris Health System. “Our success so far has not come easy or cheap. You have suffered much in terms of sickness, lost lives, lost wages, lost business and unimaginable emotional and psychological stress over these past few weeks. Because of all your sacrifices, we are now at a point that we can realistically talk about reopening our economy and return to life as we once knew it—or something close to it. … But I also want to ask you to please, remain vigilant and on guard.”
Porsa reiterated the importance of staying home, social distancing, proper hygiene, wearing masks and supporting the contact tracing work throughout the public health sector.
Shah addressed contact tracing and said the county is asking every individual to support those efforts through awareness and cooperation.
“Keep notice a bit about who you’re around,” the county’s health authority said. “Because, if three days from now you test positive and we contact you to say, ‘Hey, who have you been around,’ and you don’t remember, that makes our job extremely difficult in public health. And so, we’re asking you to be thinking about that. That really helps all of us.”
Marc Boom of Houston Methodist announced that last week more than 80 churches signed a pledge to refrain from returning to in-person worship if there are more than 50 individuals gathered throughout the month of May. He also spoke about the safety of hospitals throughout the Texas Medical Center, noting reports that individuals with urgent conditions have been avoiding necessary care for fear of exposure to COVID-19 in a health care setting.
“Now is a time to start providing care back to people who need urgent care that has been deferred,” Boom said. “We know we can do that safely and we don’t want to have a second tragedy of people having illnesses and suffering because they’re not seeking care.”
Klotman of Baylor College of Medicine added that because of advancements in genome sequencing, researchers have been able to track specific origins of the viruses infecting local individuals. He reiterated that ongoing infections are originating through community spread and not coming from inside hospitals. Klotman also named multiple hospitals in the Texas Medical Center that participated in the clinical trial for remdesivir, which is the first clinical trial that shows promise for that drug in treating COVID-19.
“It’s a very well-established scientific principle: It interferes with how the virus replicate,” Klotman said. “We got a very positive signal from that and so there’s real reason to be optimistic that at least we’re beginning to have a therapeutic that works.”
He reassured the public that the TMC’s academic medical centers continue to work on new discoveries and treatments and will participate in every promising therapy that arises. — Alexandra Becker
UPDATE | April 30, 2020, 4:45 p.m.: With Phase 1 of Gov. Greg Abbott’s plan to restart the state’s economy taking effect tomorrow, many restaurants and retailers will be begin reopening their doors. Houston Mayor Sylvester Turner and Houston’s COVID-19 Recovery Czar Marvin Odum announced measures they’re taking in order to safely and responsibly reopen the city.
“The virus has spread like fire. The curve is flattening, that is clear, but we are still reporting these new cases,” the mayor said during his daily briefing this afternoon. “Like a fire, you can extinguish the flames, but often it continues to smolder. The reality is, if you start coming back together, not engaging in social distancing, not wearing face coverings, then it’s almost like adding fuel to the fire. You may think it’s out, but quite frankly, it’s not. It will come back … with a vengeance and be reignited, so please, as we start tomorrow, May 1, for those businesses opening up in stages, be very careful.”
Although the “Stay Home Work Safe” expires today, Turner said he is modifying the order. All city permitted and sponsored events will be canceled or rescheduled through the end of May. In addition, the Houston Public Library System will remain closed through the end of the month.
As people transition back to business mode, people should continue to practice social distancing, wear face coverings and stay at home, he emphasized.
Restaurants and retailers are required to limit their occupancy to 25 percent during the first phase of Abbott’s executive order. However, Turner said the city will be relying on an honor system to make sure businesses adhere to the occupancy limit.
“Quite frankly, it’s going to be on a trust basis and self-policing because we simply don’t have the resources to be going all around the city of Houston to check whether or not you’re following the 25 percent occupancy limit,” Turner said.
During the press conference, Odum highlighted three main priorities he will be tackling in his role: testing, contact tracing and “safe zone” measures.
“We’re moving forward with a different strategy on testing in the city,” Odum said. “The situation now allows us to look at this entire geography, think about all the risks that are out there—starting with our vulnerable and at-risk communities, thinking about that from a socioeconomic standpoint, where we’ve seen outbreaks in the past … to understand where the priorities are.”
Odum and his team have developed a plan for a number of different sites around the city to make testing available and more convenient starting next week.
However, testing alone is not enough, he said.
“The reason you need these [testing and contact tracing] together is because testing identifies additional infections out there,” Odum said. “Contact tracing allows you then to contain that to a small area, so you don’t get wide community spread.”
The third priority is to track hospital bed numbers, ICU capacity and critical equipment supplies to make sure the health care system remains in the “safe zone” as the city goes through the reopening process.
Odum collaborated with the Greater Houston Partnership and chambers across the city to develop a “Reopen Houston Safely” strategy, a set of guidelines and best practices for businesses to incorporate into their operations.
The city has also distributed approximately 120,000 face coverings and masks this past week through various channels, including city council members and faith-based community organizations. Turner said he plans to distribute 50,000 to 70,000 more over the next few days.
“As we move forward, people will be assuming a little bit more risk as people come together, but we’re going to do everything we can within our power to keep everyone safe and make this reopening work,” the mayor said. “It’s going to require all of us to be responsible.” — Shanley Pierce
UPDATE | April 29, 2020, 1:30 p.m.: Mayor Sylvester Turner, along with the Texas Division of Emergency Management and the Houston Health Department, announced free COVID-19 testing in the Sunnyside community starting today and running through May 3. Sunnyside, which sits south of downtown Houston, is a predominantly African American community.
“We have other COVID-19 testing sites across the city, and this one will bring vital COVID-19 testing resources closer to vulnerable communities,” Turner said at a press conference in Sunnyside. “The test becomes our eyes in terms of where this virus is.”
Located at Worthing High School, 9215 Scott Street, the new mobile testing site will provide 150 tests daily. To make an appointment, which is required at this site, visit txcovidtest.org or call 512-883-2400.
“I am the representative for this area,” said U.S. Rep. Al Green, of the 9th Congressional District, at the press conference. “Although today we’re here at Sunnyside, this is really bigger than Sunnyside. Because what happens in Sunnyside can impact the east, west, north and south sides. … We must concern ourselves with what happens to others because it could happen to us.”
Other city officials offered updates at the press conference, as well.
The Houston Fire Department has seen a decrease in total call volume by about 20 percent since COVID-19 arrived in Houston, according to David Persse, M.D., physician director for EMS for the city of Houston and the medical director for the Houston Fire Department.
“We are seeing a slight decrease in the number of heart attacks that people are calling 911 for, as well as strokes,” Persse said. “This virus does seem to affect the blood and cause clotting—and clots can cause heart attacks and strokes. … If you think you’re having the signs and symptoms of a heart attack or a stroke, you need to call. … This virus is insidious. Please take advantage of the testing.”
Houston reported 96 new cases of COVID-19 today, bringing the total number of cases to 3,515.
The city is also reporting two more deaths related to COVID-19, bringing the total count to 52. One of the deceased was a Hispanic female in her 90s who died on April 15 and had underlying medical conditions. The other fatality was a Hispanic male in his 70s who died on April 24, also with underlying medical conditions.
“We know that African Americans and Hispanics, along with the elderly and people with underlying chronic health conditions, are disproportionately getting sick and dying from COVID-19,” Turner said. “Hispanics and African American are making up pretty much 70 or 75 percent of the 52 that have passed away.”
The curve is flattening, he added, but Houstonians must remain vigilant of the spread of the virus.
“The fight to end the pandemic is not over and our work is not done,” Turner said. — Maggie Galehouse
UPDATE | April 28, 2020, 7:30 p.m.: Houston and Harris County officials have crafted a response to Gov. Greg Abbott’s plan to reopen parts of the Texas economy on Friday aimed at avoiding a local increase in COVID-19 infections, hospitalizations and deaths.
Harris County Judge Lina Hidalgo and Houston Mayor Sylvester Turner expressed concern about backsliding on the progress of containing the virus amid local orders that have kept people at home, working safe, at physical distance and, this week, guided to wear facial coverings in public. Both executives warned of potentially perilous circumstances with more movement in the community as the virus continues to circulate.
At a Tuesday morning news conference, Hidalgo announced a three-point “test, trace, treat” plan to contain the spread of COVID-19 as parts of the Texas economy—retail stores, restaurants, movie theaters and malls—can reopen with restrictions on May 1.
In addition to strike teams for congregate care facilities, such as nursing homes, which were announced Monday, the county is opening more mobile testing sites with enhanced testing capacity, increasing tracing of positive cases and continued monitoring of hospital capacity.
“As the epicenter of COVID-19 in Texas, we in Harris County can’t take our eye off the ball,” the county judge said. “We’re not through this. … The idea is to open the economy and keep it open. If we are not smart in the way we do this, we risk a spike or—at worst—a second surge higher than the first one like they’ve seen in other countries and we risk having to go back to where we started and we risk losing all of the profound sacrifices that people have made to get us to this point.”
Harris County will expand its COVID-19 workforce by recruiting about 300 “contract tracers”—employees and volunteers who will reach out to people who have come into contact with someone infected to ensure those individuals get tested and isolate for two weeks to prevent further spread of the virus.
“In order to test all the new cases and their contacts with existing resources for us to be safe, it is imperative that we keep the new cases per day below 100,” Hidalgo said.
The county judge also noted that the curve for area hospital admissions is flat, but there continue to be about 200 admissions a day.
“If we tripled every seven days like we were doing early in our curve, that would quickly run out of capacity,” she said, noting plans for a makeshift hospital if local health care centers become overwhelmed.
Data on the infection rate, ICU beds, ventilators and other metrics for Texas Medical Center-affiliated institutions in nine counties can be found in the TMC’s daily situation report.
During an afternoon news conference at Fonde Community Center near downtown Houston, which has been opened as an ancillary shelter for 150 homeless individuals, Turner responded to the governor’s order and announced city efforts to serve the homeless during the COVID-19 crisis. The mayor also bemoaned the possibility of the state action undercutting the city’s successful early prevention efforts. He noted that all programs and events produced, permitted and sponsored by the city are on hold until the end of May. As well, city libraries will remain closed through the month of May.
“We all want to be back to some sense of normalcy, but I think it’s very important that we do it in a very judicious fashion,” Turner said. “Just because something opens up doesn’t necessarily mean you have to go in there. … As long as we are reporting new cases and as long as we are reporting people who are dying and as long as we can’t tell you that this virus is out of here, then you need to be very, very, very, very careful.”
The city repurposed funding for the Fonde shelter, operated by The Salvation Army, to allow the largest emergency shelters to decompress and institute social distancing. There is now a homeless testing hotline at 713-286-6047 for service at Healthcare for the Homeless-Houston.
The city has provided more than 20 handwashing stations in areas with a high concentration of homeless individuals and has distributed masks, sanitizer and antiseptic wipes to homeless persons and the agencies that serve them.
In addition, there is now a city-county quarantine facility with food and medical care for 126 homeless individuals who are referred from hospitals to isolate with an expansion potential for another 60 rooms, if needed.
The respite facility and services have been coordinated with the Coalition for the Homeless—an umbrella for more than 100 organizations that comprise the homeless response system in Houston, Harris County, Fort Bend County and Montgomery County—as part of a long-term local solution to homelessness.
“When this is over … we are going to be housing more people—not less,” said Mike Nichols, the coalition’s president and CEO. “Throughout the pandemic, the coalition has been working with our partners to ensure that ongoing homeless services are able to stay operational and to stand up additional services for people experiencing homelessness.”
As of Tuesday afternoon, more than 1 million people nationwide have tested positive for the virus. There are more than 26,000 confirmed cases in Texas, 2,567 in Harris County and 3,419 in Houston. Deaths nationally have exceeded 52,000 with more than 660 in Texas, according to the Texas Department of State Health Services, including 53 in Harris County and four new confirmed fatalities in Houston for a total of 50 in the city. — Cindy George
UPDATE | April 27, 2020, 4:20 P.M.: Earlier this afternoon, Gov. Greg Abbott announced his tiered plan to reopen Texas.
After the state stay-at-home order expires on April 30, the first phase of Abbott’s strategy will allow retail stores, restaurants, movie theaters and malls to reopen on May 1 at no more than 25 percent capacity. Museums and libraries also will be allowed to reopen their doors, but all hands-on exhibits must remain closed.
Outdoor sports that keep a certain distance, such as golf and tennis, will be allowed but limited to no more than four people at a time.
Phase 2 of Abbott’s plan could go into effect as soon as May 18.
“Phase 2 will open more businesses and allow the businesses open in Phase 1 to expand their operations. We need to see two weeks of data to confirm no flare-up of COVID-19,” Abbott said. “That is exactly why now, more than ever, Texans must continue safe distancing practices. If we do that, we will be able to expand into Phase 2, opening up our economy even more.”
Barbershops, hair salons, bars and gyms will remain closed for now. The governor said he is aiming for “on or no later than mid-May” to reopen those businesses.
Abbott’s executive order supersedes orders set at the local level.
A screenshot of Gov. Greg Abbott during his press conference on Monday, April 27, 2020.
During Houston Mayor Sylvester Turner’s regular daily briefing, held shortly after Abbott’s news conference, Turner commented on the governor’s plan to reopen, saying “there are still things we need to do.” Turner emphasized the need for more widespread testing to better understand where the virus that causes COVID-19 is circulating and “whether or not we’re getting our arms around this virus.”
There are 74 new COVID-19 cases and 4 new deaths in the city of Houston, bringing the total to 3,358 cases and 46 deaths.
“The key to stopping the community spread of the coronavirus in our city is in our practice of social distancing, good hygiene, wearing face coverings … and testing, testing, testing,” Turner said. “It’s testing for the city of Houston that we will continue to focus on and place a great deal of emphasis on. I know people want to open up. I got that. I understand that, but what drives me as the mayor of Houston at this point … is local cases more prevalent in at-risk neighborhoods.”
Earlier Monday, Turner announced a new COVID-19 testing site for the Gulfgate area, which has more vulnerable and high-risk populations.
Located at the Barnett Sport Complex, the United Memorial Medical Center testing site is open to everyone—with or without symptoms—at no cost.
“It is important for us to know who has it and who doesn’t have it in order to send people back to work in a safe and responsible way,” Turner said.
Harris County Judge Lina Hidalgo announced this morning two additional testing initiatives to combat COVID-19: the formation of a countywide testing strike team and the opening of two additional pop-up testing locations.
Beginning April 28, the strike team—which will include county epidemiologists, public health experts, social workers and testing staff—will be deployed to congregate care facilities at high risk of COVID-19 spread to perform site assessments, make recommendations or issue control orders as needed. The strike team will start with one nursing home a day at first, then expand to other facilities, such as senior centers and shelters.
“In some ways these facilities are the path of least resistance for the virus,” Hidalgo said during her news conference, adding that folks who live in homeless shelters and senior living facilities “are sitting ducks right now and we can’t allow that.”
Hidalgo also noted that she is doubling the number of pop-up or mobile testing sites from two to four.
Two mobile sites will be located in Tomball and southeast Houston on Monday and Wednesday, then move to southwest Houston and Crosby from Thursday through Saturday. The locations of the other two mobile sites will be announced later.
Each mobile testing site has the capability to test up to 150 individuals per day. The two fixed sites in Katy and Baytown each can test up to 500 daily. — Shanley Pierce
UPDATE | April 24, 2020, 4:45 p.m.: The Houston Health Department (HHD) reported 74 new cases of COVID-19 on Friday, bringing the total to 3,120.
HHD also reported one new death due to COVID-19, bringing the city’s total coronavirus fatalities to 35. This was the first death recorded after four consecutive days with no fatalities.
“The one new death is a white non-Hispanic male in his 70s with no known underlying health condition,” said Mayor Sylvester Turner at a Friday press briefing. “This is the first time we are reporting the death of someone with no known underlying health conditions.”
Data from Houston’s hospital systems suggests that the in-hospital population of individuals diagnosed with COVID-19 has flattened, said David Persse, M.D., the city’s health authority.
“We’re not coming down yet. We’ve plateaued. We are right now at the same pace as the power of this virus,” Persse said, adding that citizens should continue to wear masks and practice social distancing. “Don’t take your foot off the brake. It’s working.”
Starting Monday, Gulf Coast Regional Blood Center (GCRBC) will begin taking plasma from individuals who tested positive for COVID-19 and recovered. Volunteers must have documented proof of a positive test; the center will work with them to make sure the infection is gone. Studies have shown that antibodies in the plasma of recovered COVID-19 patients may help critically ill COVID-19 patients recover. The plasma is administered via transfusion.
“It takes less than an hour to give plasma,” Persse said. “It’s no more difficult than giving blood.”
Volunteers interested in donating plasma can get more information at the GCRBC website, giveblood.org, or by calling 713-791-6608 starting Monday, April 27.
The city’s newly-formed Health Equity Response (HER) task force has already received its first shipment of 50,000 masks and distributed them throughout the city. HER is designed to bring information and supplies to those most at risk and disproportionately affected by COVID-19. The task force plans to distribute more than 200,000 masks, Turner said.
The recently-formed Mayor’s Office for People with Disabilities (MOPD) Food Assistance Program will expand deliveries being made directly to people’s homes. The program will deliver food to 1,000 households per week for the next two weeks.
“We are asking the community to be patient,” said Gabe Cazares, MOPD director. “We are working as quickly as possible.”
Members of the Houston Health Department and volunteers from the Houston Fire Department are visiting more than 300 nursing homes and assisted living centers to provide COVID-19 education and assistance to residents and employees, including screening and monitoring. Getting ahead of the virus will help prevent the spread of COVID-19 among the most vulnerable, city officials said. — Maggie Galehouse
UPDATE | April 23, 2020, 5:45 p.m.: Mayor Sylvester Turner announced today during an afternoon press conference that the Houston Health Department reported 71 new cases of COVID-19, bringing the city’s total to 2,346. There were no deaths today, marking the fourth consecutive day that Houston has reported no fatalities from COVID-19.
Houston METRO Board Chair Carrin Patman shared how the Houston METRO is working to protect its employees and riders during the pandemic. Ridership has dipped in all sectors but less for the TMC and its park and rides. The transit authority has implemented social distancing practices on buses, suspended fares, initiated temperature checks when employees arrive to work and will be supplying masks to riders as available.
Turner stressed the importance of wearing masks to comply with the new order from Harris County Judge Lina Hidalgo, effective Monday, April 27. Joining the press conference virtually to add their support to the Mask Up Houston campaign (#MaskUpHOU) were Olympic gold medalist Simone Biles, Houston Astros shortstop Carlos Correa and local rapper Slim Thug.
“If you do have to leave the house, I would strongly suggest that you mask up and glove up and just sanitize on the regular,” said Slim Thug, who has made a full recovery from COVID-19.
Turner emphasized that his goal was to provide masks rather than simply enforce the order, saying the city should not have a mandate without providing adequate resources.
“Masks over citations,” Turner said. “We don’t give citations. We give masks or face coverings.”
To support the city’s most vulnerable communities, Turner announced a new Health Equity Response task force that will focus on bringing more information and more supplies to those most at risk and disproportionately affected by COVID-19. Strategies include a public health education campaign to encourage residents in the highest risk neighborhoods to take additional precautions to protect themselves and others; direct community support to distribute essential supplies to Houstonians, including masks; and a Houston health equity response fund to accept donations that will provide resources to those who need them most.
“Here in Houston, as in many other parts of our nation, the pandemic is magnifying the pre-existing health disparities and socioeconomic challenges facing our most vulnerable communities,” said Shannon Buggs, Complete Communities director at the mayor’s office and a member of the new task force. “Before COVID-19, we already knew that 39 percent of Houstonian households didn’t have $400 for an emergency. Now, despite stay-at-home orders, only 1 out of every 5 black workers and 1 out of every 6 Latino workers in the United States actually can work from home, compared with 30 percent of white workers and 37 percent of Asian workers. … Mayor Turner appointed the Health Equity Response task force to keep the focus on the most acute and critical needs.”
Turner also announced an initiative for members of local faith communities to help make more than 1 million masks.
“We are committed to not leaving anyone behind,” Turner said. “The City of Houston is the most diverse city in the country, and in order to make sure that we touch the needs, it is important that this team be as diverse as possible. And we are committed to doing just that. …We want to make sure that we are touching, and working very closely, with all of our communities, especially those who are at risk and are most vulnerable.”
Earlier today, Harris County Public Health (HCPH) announced its revamped COVID-19 online self-assessment tool to improve the testing process with advanced scheduling options. Testing is free and open to the public, regardless of citizenship status, but all individuals must register first and obtain a unique identification code. More information about the assessment can be found at www.readyharris.org or www.hcphtx.org or by calling 832-927-7575.
Additionally, the Texas Policy Lab (TPL) in Rice University’s School of Social Sciences has joined Hidalgo’s office in the fight against the COVID-19 pandemic. TPL is drawing upon their expertise to provide the county with relevant data, including evaluation of the effectiveness of the county’s Stay Home, Work Safe order. — Alexandra Becker
UPDATE | April 22, 2020, 6 p.m.: Harris County will require face coverings in public beginning Monday, County Judge Lina Hidalgo and Houston Mayor Sylvester Turner announced in a joint news conference.
The order applies to people 10 and older for 30 days beginning April 27 with exceptions for people with health conditions, those exercising alone or while driving and eating. Residents have been given several days to acquire or make a face covering, which doesn’t have to be medical grade, but must be a mask or other item that protects the nose and mouth. Order violators apprehended at the discretion of law enforcement agencies could face a $1,000 fine or up to 180 days in jail.
“Face coverings are not a substitute for social distancing,” Hidalgo said. “We are still under a stay home, work safe order. We should not be out unless absolutely necessary. And if we do this, we will get that curve down to where it needs to be to where we can actually begin reopening things and do so in a way that is sustainable.”
Turner noted that the city’s COVID-19 deaths remained at 34 for the third consecutive day. He also mentioned reports from the Texas Medical Center that show COVID-19 discharges outnumber current hospitalizations for TMC-affiliated institutions.
“A face covering will help slow the spread of this coronavirus and can save lives,” the mayor said. “Wearing a face covering protects other people from you because you do not know if you are a carrier and can transmit the virus. You can be asymptomatic.”
David Persse, M.D., the city’s public health authority, pressed the importance of face coverings given the predominance of “asymptomatic or pre-symptomatic or minimally symptomatic spread” and how measures taken so far have staved off the virus, which is circulating in the community, from devastating the area with illness, hospitalizations and deaths.

Texas Medical Center COVID-19 data released April 22, 2020.
“From my standpoint, the most important number for us to be watching are the hospitalization numbers,” he said. “In order to save lives, we have to make sure that if somebody needs a hospital bed, that there is a hospital bed available for them. As a community, because of the things that we have done—including wearing facial coverings, social distancing and not gathering in large groups–we have been, actually, quite successful. … The overall death count in this area compared to major urban areas across the nation, per capita, is remarkably low. That’s because of the things that we have been doing. It’s not in spite—it is directly because of.”
Harris County Public Health Executive Director Umair Shah, M.D., MPH recognized Wednesday as Earth Day and advised against improperly disposing of protective items such as gloves by throwing them on the ground.
“Don’t litter. Don’t ruin our community,” he said. “We are making progress.” — Cindy George
UPDATE | April 21, 2020, 4:30 p.m.: Mayor Sylvester Turner on Tuesday announced a food assistance program for people with disabilities that will deliver food and other items directly to the homes of individuals who are unable to get to food distribution centers as a result of the COVID-19 crisis.
“There are food insecurities in our city,” Turner said. “We do not want to leave anyone behind.”
Gabe Cazares, director of the Mayor’s Office for People with Disabilities, explained that the MOPD Food Assistance Program was made possible by the city’s community partners at Walmart, Sam’s Club, the Houston Food Bank and Houston Metro.
“We are so grateful for our partners,” Cazares said. “Walmart and Sam’s Club contributed about $30,000 worth of goods and the Houston Food Bank has made a substantial contribution, as well.”
Houston Metro will deliver boxes to people’s homes that include sealed food that can be stored at room temperature, fresh produce and basic home necessities. The boxes are being assembled at the city’s West End Multi-Service Center over the next few days. Deliveries will begin on Friday, April 24.
To access the program, visit houstontx.gov/disabilities or call 832-394-0814.
Mayor Turner also reported 20 new COVID-19 cases today in Houston and zero deaths related to the disease caused by the novel coronavirus. This is the second consecutive day the city has reported no COVID-19 deaths. — Maggie Galehouse
UPDATE | April 20, 2020, 4 p.m.: Houston Mayor Sylvester Turner and Harris County Judge Lina Hidalgo announced in separate news conferences Monday the appointment of two relief and recovery czars focused on the long-term effects of the COVID-19 crisis. Turner named Marvin Odum, the former president of Shell Oil, to lead recovery efforts for the city of Houston. Hidalgo appointed State Rep. Armando Walle to lead recovery efforts in Harris County.
Marvin Odum, who was named the COVID-19 relief and recovery czar for the city of Houston, speaks Monday at Mayor Sylvester Turner’s press conference.
“This is about keeping people safe, getting people back to work and recharging our economy,” Odum said at Turner’s gathering.
Odum, who served as chief recovery officer for the city after Hurricane Harvey, identified four key areas of focus: determining how testing and contact tracing for COVID-19 can be applied to a back-to-work plan that develops and sustains confidence among Houstonians; identifying problems that may arise and making the necessary adjustments with speed and transparency; working with the federal government to spend federal and local money wisely; and developing a plan to address future viral attacks on the city.
Odum said he and Walle would be “working hand-in-hand to represent the people of Houston and Harris County.”
Both czar roles are unpaid, volunteer positions.
In a morning briefing, Hidalgo explained her appointment of Walle, who represents District 140 in the Texas Legislature.
“We need someone who will be laser-focused on helping families right now and combatting the long-term economic effects and the long-term human impacts of this crisis,” Hidalgo said. “Our goal of this is to make sure our relief and recovery is inclusive, fast and coordinated.”
Judge Hidalgo also noted that her appointment of Walle was, in part, because of his experience working in underserved areas.
“He represents the Aldine area and knows the struggles that families in unincorporated Harris County face every day,” Hidalgo said.
Walle, who spoke briefly at the press conference, said the effort will be inclusive and collaborative.
“We expect to work with a wide variety of reasonable stakeholders in this effort, including from the private sector, philanthropy, faith-based organizations, nonprofits and local governments—from the City of Houston to all our smaller municipalities—and including our unincorporated part of the region, which is about over two million people in unincorporated Harris County,” Walle said. “We need to work together on an inclusive recovery that responsibly insures the health and economic well-being of the people of Harris County. We need to save lives and also save livelihoods.”
Hidalgo also noted that the crisis is by no means over but that the curve in the Greater Houston Area is flattening because of social distancing measures.
“We’re not out of the woods, so we’ll continue to go through this information together, but essentially, you can see the intake’s flat, and if we all do our part, eventually that will fall down and we’ll all be in a place to begin lifting our restrictions. But how quickly we do that will depend on each of you to continue to stay home so that that curve actually hits its peak and lowers,” Hidalgo said. “If we work together now, the sum of each of our parts is what’s going to get the economy back on track.”
Harris County Public Health (HCPH) Executive Director Umair Shah, M.D., MPH, also spoke at Hidalgo’s news conference, noting that the county has expanded testing criteria to individuals who are asymptomatic but believe they may have come into contact with someone positive for COVID-19. He said HCPH encourages individuals to get tested in an effort to gain a better understanding of the disease’s scope throughout the Houston region.
Although the fatalities in Houston did not rise on Monday—total deaths remain at 34—the Houston Health Department reported 107 positive COVID-19 cases for a total of 2,923. — Alexandra Becker and Maggie Galehouse
UPDATE | April 17, 2020, 5:30 p.m.: On Friday, Texas Gov. Greg Abbott announced three executive orders that will begin the process of reopening the state.
“Because of the efforts of everyone to slow the spread, we are now beginning to see glimmers that the worst of COVID-19 may soon be behind us,” Abbott said during a press conference earlier this afternoon.
The governor’s executive order established the Statewide Strike Force to Open Texas, which includes Lt. Gov. Dan Patrick, House Speaker Dennis Bonnen, Attorney General Ken Paxton and Comptroller Glen Hegar, along with a team of state health experts and business leaders, to gather information and make recommendations regarding the process and safe practices for businesses to follow in order to safely reopen.
With Texas boasting the second-most recoveries from COVID-19 of all states in the country, Abbott said he plans to take a cautious, staged approach to reopening.
As part of Abbott’s executive order, state parks will reopen Monday, April 20 with new visitor guidelines. All visitors are required to wear face coverings or masks, must stand six feet away from people who are not within the same household and are prohibited from gathering in groups larger than five.
Effective Wednesday, April 22, current restrictions on nonessential medical procedures will be loosened to allow doctors, nurses and medical staff to perform procedures, such as cancer diagnostic testing.
Starting Friday, April 24, all retail stores in the state should be able to operate “retail-to-go,” allowing customers to place orders online and pick up products or have them delivered while minimizing contact, Abbott said.
“We’ve shown that we can both continue our efforts to contain the coronavirus, while also adopting safe standards that will allow us to begin the process of reopening business in Texas,” Abbott said. “Because we’ve seen that this model works, while also containing COVID-19, we believe all stores in Texas should be able to operate retail-to-go beginning next Friday.”
In addition, all classrooms will remain closed for the remainder of the 2019–2020 school year.
More details about the governor’s plan to reopen Texas will be announced on Monday, April 27.
While Houston Mayor Sylvester Turner has yet to unveil his plans to reopen the city, he stressed the importance of a “measured approach.”
“The last thing I would want to do … is to change course too quickly and we end up seeing things starting to spike,” Turner said during his daily press conference this afternoon, shortly after Abbott’s announcement. “If we take our foot off the brake, we can easily start moving back in the other direction.”
On Monday, Turner plans to announce a local leader who will help lead the city’s recovery as well as provide more information about plans to reopen. For now, he said he anticipates some restrictions will remain through the end of May, especially city operations and the cancellation of city-sponsored and permitted events, in order to stop the spread of COVID-19 in Houston.
As of today, there are 114 new cases in Houston, bringing the total to 2,570 confirmed infections, and 31 deaths.
“We are still going through this storm, and we are not yet out of the storm,” Turner said. “I know Gov. Abbott made an announcement earlier today about phasing in the reopening of Texas. I certainly look forward to hearing more of the details. We are assessing, even now, the things he had to say and his executive orders.” — Shanley Pierce
UPDATE | April 16, 2020, 4:30 p.m.: The City of Houston received a $100,000 grant and 10,000 diagnostic testing kits from Hyundai Motor America to allow for the expansion of diagnostic testing in the city to combat COVID-19.

U.S. Rep. Sheila Jackson Lee presents a check of $100,000 to Houston Mayor Sylvester Turner as part of a grant from Hyundai Motor America to support efforts combatting COVID-19.
“We know that the state of Texas has not fared well in testing—14,624 cases … and 318 deaths—but it matters to us that we continue to work,” U.S. Rep. Sheila Jackson Lee said during Mayor Sylvester Turner’s daily briefing this afternoon. “There are people now as we stand here today that are in hospitals fighting for their lives in Houston and Harris County. Many of those were not tested. We do not want that to be our future. We’re sad that it is our past.”
The grant and testing kits, valued at approximately $150,000, will go to the Houston Health Foundation, which supports the work of the Houston Health Department.
“We continue to recognize the need for expanding testing throughout Houston and Harris County, and this grant will allow us to work with a variety of community-based organizations to further that goal,” Turner said. “It is imperative that we expand into neighborhoods, given the Houston Health Department’s directive to do exactly that.”
Houston was one of several cities Hyundai selected—including Chicago, Detroit and New Orleans—to receive the gift, which is part of the automaker’s larger effort to provide $4 million in grants to support COVID-19 drive-through testing to 22 hospitals nationwide, as well as 65,000 testing kits, through its Hyundai Hope On Wheels program.
While the White House released new guidance this afternoon that outlines the process for states to reopen in an effort to resuscitate the hard-hit economy, Turner said he and local officials are working on next steps, but “are not at this point ready to announce how we are going to open the city up. Those announcements and pronouncements will come, but not today.”
The mayor emphasized continuing with current public health and government orders.
“We are focusing right now on making sure that people are staying at home, working safely, engaging in social distancing and wearing face coverings because we are still in this storm,” he said. “I want people to be singularly focused on doing everything we can to keep themselves safe and to keep other people safe.” — Shanley Pierce
UPDATE | April 15, 2020, 4 p.m.: Houston Mayor Sylvester Turner reported 52 new cases of COVID-19 in Houston, for a total of 2,331 cases.
Houston Mayor Sylvester Turner conducts a press briefing on April 15.
In all, 26 individuals have died of COVID-19 in the city, Turner said at his daily press briefing, a tally that includes three newly reported deaths: an African American man in his 80s, an African American man in his 60s and a white, non-Hispanic man in his 50s. All three individuals suffered from underlying health conditions, the mayor said.
The race/ethnicity breakdown of Houston’s 26 COVID-19 deaths, according to the Houston Health Department:
Black/African American (non-Hispanic): (14) 54%
Hispanic/Latino: (6) 23%
White (non-Hispanic): (6) 23%
Elizabeth Killinger, president of NRG Retail and Reliant, announced a donation of $300,000 to Houston’s first responders and health care workers. Half will go to the city’s new Houston Frontline Fund, to provide personal protective equipment (PPE) to the Police and Fire Department, Health Department and other essential personnel covering COVID-19 testing sites. The other $150,000 goes to the Greater Houston COVID-19 Recovery Fund, a collaboration between the United Way of Greater Houston and the Greater Houston Community Foundation.
A Houston Health Department analysis of COVID-19 deaths by jurisdiction, per 100,000 people, showed a comparatively low total for Houston, the mayor said. New York City has had 94.1 deaths per 100,000 people; New Orleans has seen 70.6 deaths per 100,000 people; Chicago has suffered 12.8 deaths per 100,000 people; and Houston has seen 1.1 COVID-19 deaths per 100,000 people.
Talks with Texas Medical Center leaders have been optimistic, Turner said. “As of today,” he said, “hospitals in our area can handle cases coming in at baseline capacity.”
The mayor closed the press briefing with a few words on the census. A little more than 40 percent of Houstonians have responded to Census 2020, the mayor said. He encouraged people to take the time to fill out their census forms, as a complete count will help lock in the proper resources and representation for myriad public health issues over the next 10 years. — Maggie Galehouse
UPDATE | April 14, 2020, 7:30 p.m.: As the city’s drive-through testing capability doubles this week, there’s also a new program providing a small number of COVID-19 tests in the homes of challenged individuals.
A city partnership with Houston innovation company imaware will offer 250 free at-home tests.
“We are identifying people who are in particular situations where there is no way they can get tested any other way and they have a need. We are referring them to imaware,” David Persse, M.D., the city’s health authority, said during the mayor’s news conference today. “We have 250 of them in a population of 2.5 million people. It’s a tiny number and we are trying to be very strategic with it.”
The people tested in their homes have been seniors 60 and older and persons with disabilities, Letosha E. Gale-Lowe, M.D., the Houston Health Department’s chief physician, said in a phone interview. When an individual calls the city’s COVID-19 hotline at 832-393-4220, a screener determines whether the person is eligible for in-home testing.
“A lot of times those folks require a lot of intensive resources to get them to a test site,” she said. “This is for those really, really vulnerable persons who need the testing, are most susceptible to the complications but just cannot get out—and their families can’t get them out.”
The nasopharyngeal swabs are administered by imaware personnel with results in 48 hours. Over the last two weeks, about 10 people have been tested at home, Gale-Lowe said.
Houston Mayor Sylvester Turner said city officials are working to increase the number of test kits available beyond the two drive-through testing sites and the imaware program.
“If things go well, we can have some announcement on that within the next couple of days,” the mayor said. “We are looking at partnering with the private sector to really ramp up and expand the amount of testing that we can do.”
As of Tuesday afternoon, there were more than 600,000 confirmed COVID-19 cases nationwide with more than 14,600 confirmed cases in Texas, greater than 1,500 in Harris County and 2,279 in Houston. Deaths nationally have exceeded 25,000 with 318 in Texas, according to the Texas Department of State Health Services, including 29 in Harris County and 23 in Houston.
All of Houston’s COVID-19 fatalities were individuals with underlying conditions. The city is also including race and ethnicity demographics to note that 12 of the 23—52 percent—were black patients. That means African Americans, who comprise about 23 percent of Houston’s population according to U.S. Census Bureau estimates, are bearing a disproportionate, roughly double, burden of disease, according to the data. — Cindy George
UPDATE | April 13, 2020, 7 p.m.: With an increasing capacity to provide twice as many tests every day, the city’s COVID-19 testing sites are open to everyone now without the previous requirement of symptoms, Mayor Sylvester Turner announced today.
“We will begin offering testing to anyone who wants it, not just those who are showing symptoms,” he said. “Whether you are symptomatic or asymptomatic … you will be eligible to get testing. This will give us a better idea of community spread in the city of Houston.”
Those seeking testing must still contact the Houston Health Department’s COVID-19 call center at 832-393-4220 between 9 a.m. and 7 p.m. to receive a unique ID code with details about where to go for testing and how to obtain results. Those who show up without this code will not be tested.
City testing sites have been providing 250 tests daily at each location, but will be increasing volume to offer 1,000 every day via 500 tests at each site.
Two new mobile units will provide drive-through testing at pop-up sites that will rotate across Harris County precincts starting Tuesday, County Judge Lina Hidalgo announced. Each site will be able to test 100 people daily which adds 200 tests per day. This augments a pair of Harris County Public Health stationary sites. They will increase capacity to 500 tests per location—1,000 daily combined—starting Wednesday.
A new private testing site on Houston’s south side at Cullen Middle School, 6900 Scott Street, opened today between the South Park and Sunnyside, which the mayor called a “vulnerable community.”
David Persse, M.D., the city’s health authority, said people with symptoms remain the top testing concern because they “push the virus through the community” but asymptomatic people can receive a false positive yet have COVID-19, so social distancing remains an important preventive public health action.
Reliable and robust testing as well as data on COVID-19 hospital admissions and deaths is vital information that officials will use to make decisions in the future, Persse said during the news conference.
A new daily dashboard now available at tmc.edu, the Texas Medical Center’s corporate website, provides updated data on the availability of ICU beds, ventilators, personal protective equipment and other pandemic metrics for TMC institutions operating across nine Houston-area counties. Those TMC affiliates are CHI St. Luke’s, Harris Health System, Houston Methodist, MD Anderson Cancer Center, Memorial Hermann and Texas Children’s Hospital. Facilities operated under other brands are not included in the data.
As of Monday afternoon, there are 579,000-plus cases nationwide, more than 13,900 confirmed cases in Texas, greater than 1,500 in Harris County and 2,239 in Houston. Deaths nationally have exceeded 23,000 with 287 in Texas, according to the Texas Department of State Health Services, including 28 in Harris County and 18 in Houston. The city is reporting that all COVID-19 fatalities were individuals with underlying conditions and are also including race and ethnicity demographics to note that 10 of the 18 were black patients. — Cindy George
UPDATE | April 10, 2020, 6:45 p.m.: To discourage holiday gatherings such as Easter Egg hunts and enforce social distancing, Harris County and Houston parks are closed this weekend.
The city announced two additional COVID-19 deaths on Friday, bringing Houston’s reported total to 16. The city is also reporting race/ethnicity demographics on the deceased, which are now 56 percent black, 25 percent Hispanic and 19 percent Anglo.
A new daily dashboard now available at tmc.edu, the Texas Medical Center’s corporate website, provides updated data on the availability of ICU beds, ventilators, personal protective equipment and other pandemic metrics for TMC institutions operating across nine Houston-area counties. — Cindy George
UPDATE | April 9, 2020, 5:30 p.m.: There’s hope and speculation about whether the virus that causes COVID-19 will wane in warmer temperatures.
“I don’t know if it’s seasonal or not, but if there’s any place that’s going to find out, it’s going to be Houston, so let’s hope it is sensitive to the weather,” said David Persse, M.D., the city’s health authority said during a mayor’s news conference this week.
A “rapid expert consultation” sent to the White House Office of Science and Technology Policy from the National Academies of Sciences, Engineering, and Medicine as well as from the organizations’ Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats said hotter weather significantly diminishing the virus is unlikely, according to a story in The Washington Post.
The “seasonal variation” is unknown, but “some limited data support a potential waning of cases in warmer and more humid seasons,” the eight-page report said, adding that ongoing studies “as the pandemic unfolds could shed more light on the effects of climate on transmission.” — Cindy George
UPDATE | April 8, 2020, 4 p.m.: CDC releases COVID-19 contact tracing case study
The Centers for Disease Control and Prevention (CDC) has published a case study on community transmission of SARS-CoV-2, the virus which causes COVID-19 disease, at a funeral and a birthday party in Chicago.
“Community Transmission of SARS-CoV-2 at Two Family Gatherings — Chicago, Illinois, February-March 2020” published today in the CDC’s Morbidity and Mortality Weekly Report (MMWR) focuses on contact tracing, which is the monitoring of individuals potentially exposed to an infectious disease.
According to the World Health Organization (WHO), contact tracing is defined by three critical steps: contact identification, contact listing and contact follow-up.
Contact identification includes determining all individuals an infected person has been physically near since the onset of illness. Contact listing includes informing those contacts about their possible exposure and providing information about the disease as well as protocol to minimize further spread. Contact follow-up is regular communication with all contacts for the purpose of monitoring for symptoms and testing for signs of infection.
The report is one of the first significant illustrations of how SARS-CoV-2 has spread throughout a community in the United States beyond household contacts, health care workers and residential facilities.
On average, there were four days between contact with an infected individual and the onset of symptoms.
During February and March, the Chicago Department of Public Health investigated a “large, multifamily cluster” of individuals with confirmed COVID-19 disease and their close contacts. The study illustrates 16 cases of confirmed or probable COVID-19 disease, including three deaths—all of which are believed to originate with a single individual (see A1.1 in the chart)—that spread at two different gatherings. The virus caused illness beyond the original infected contacts through additional activities, which included providing care for one of the infected individuals, household exposure, a hospital visit and attending church. The chart illustrates the movement of infection to and through the 16 individuals. The people in the study are referenced by their family cluster letter (A or B), then by the transmission generation (1 through 4) and finally by the sequence within each generation, indicating the order in which each individual was infected (1 through 7). Thus, the original case is A1.1.
The report reinforces the CDC’s urgent recommendations that individuals follow social distancing guidelines and stay-at-home orders to slow or stop transmission of SARS-CoV-2. — Alexandra Becker
UPDATE | April 7, 2020, 5 p.m.: Federal health partners helping at Houston’s COVID-19 testing sites will remain through April 30, said Houston Mayor Sylvester Turner during an afternoon press conference at City Hall.
Six federal employees will continue to work at the city’s two testing sites until the end of the month and “the PPEs [personal protective equipment] will continue to come and the federal government will continue to assume 100 percent of the cost,” Turner said.
The city reported 1,145 COVID-19 cases on Monday, Turner said, but only 146 of those individuals were hospitalized. “The overwhelming majority are self-isolating at home and recovering at home,” he said.
Due to high temperatures today—97 degrees in some places—Harris County Public Health closed COVID-19 testing sites at noon.